Volume 83, Issue 1
Displaying 1-50 of 79 articles from this issue
-
2013Volume 83Issue 1 Pages 1-20
Published: 2013
Released on J-STAGE: December 21, 2013
Download PDF (24608K)
Technology and instrument
-
2013Volume 83Issue 1 Pages 43-46
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (512K) -
2013Volume 83Issue 1 Pages 47-50
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (1112K)
Clinical study
-
2013Volume 83Issue 1 Pages 51-55
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (594K) -
2013Volume 83Issue 1 Pages 56-59
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (281K) -
2013Volume 83Issue 1 Pages 60-64
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (640K) -
2013Volume 83Issue 1 Pages 65-68
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (425K) -
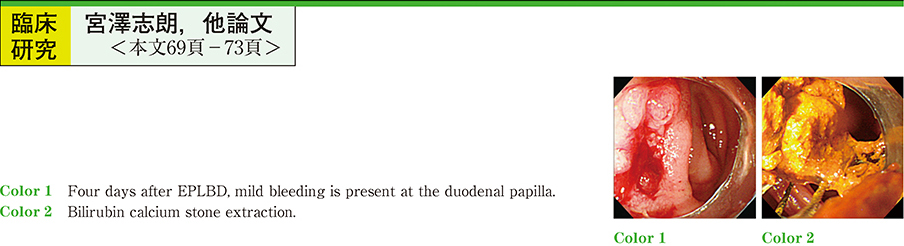
2013Volume 83Issue 1 Pages 69-73
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (612K)
experience
-
2013Volume 83Issue 1 Pages 74-76
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (350K)
Technology and instrument
-
2013Volume 83Issue 1 Pages 78-79
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (603K)
Case report
-
2013Volume 83Issue 1 Pages 80-81
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (241K) -
2013Volume 83Issue 1 Pages 82-83
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (612K) -
2013Volume 83Issue 1 Pages 84-85
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (606K) -
2013Volume 83Issue 1 Pages 86-87
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (232K) -
2013Volume 83Issue 1 Pages 88-89
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (427K) -
2013Volume 83Issue 1 Pages 90-91
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (473K) -
2013Volume 83Issue 1 Pages 92-93
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (655K) -
2013Volume 83Issue 1 Pages 94-95
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (498K) -
2013Volume 83Issue 1 Pages 96-97
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (664K) -
2013Volume 83Issue 1 Pages 98-99
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (595K) -
2013Volume 83Issue 1 Pages 100-101
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (683K) -
2013Volume 83Issue 1 Pages 102-103
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (765K) -
2013Volume 83Issue 1 Pages 104-105
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (683K) -
2013Volume 83Issue 1 Pages 106-107
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (699K) -
2013Volume 83Issue 1 Pages 108-109
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (226K) -
2013Volume 83Issue 1 Pages 110-111
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (243K) -
2013Volume 83Issue 1 Pages 112-113
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (231K) -
2013Volume 83Issue 1 Pages 114-115
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (291K) -
2013Volume 83Issue 1 Pages 116-117
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (391K) -
2013Volume 83Issue 1 Pages 118-119
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (660K) -
2013Volume 83Issue 1 Pages 120-121
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (469K) -
2013Volume 83Issue 1 Pages 122-123
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (983K) -
2013Volume 83Issue 1 Pages 124-125
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (648K) -
2013Volume 83Issue 1 Pages 126-127
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (836K) -
2013Volume 83Issue 1 Pages 128-129
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (231K) -
2013Volume 83Issue 1 Pages 130-131
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (445K) -
2013Volume 83Issue 1 Pages 132-133
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (350K) -
2013Volume 83Issue 1 Pages 134-135
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (558K) -
2013Volume 83Issue 1 Pages 136-137
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (715K) -
2013Volume 83Issue 1 Pages 138-139
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (629K) -
2013Volume 83Issue 1 Pages 140-141
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (911K) -
2013Volume 83Issue 1 Pages 142-143
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (264K) -
2013Volume 83Issue 1 Pages 144-145
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (380K) -
2013Volume 83Issue 1 Pages 146-147
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (745K) -
2013Volume 83Issue 1 Pages 148-149
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (645K) -
2013Volume 83Issue 1 Pages 150-151
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (744K) -
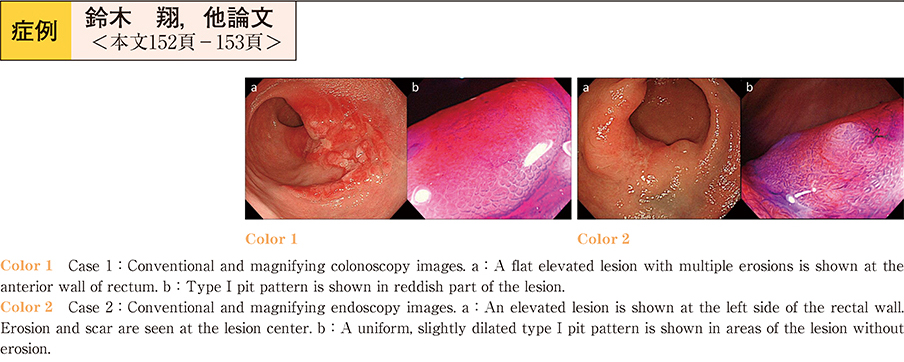
2013Volume 83Issue 1 Pages 152-153
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (574K) -
2013Volume 83Issue 1 Pages 154-155
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (1242K) -
2013Volume 83Issue 1 Pages 156-157
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (506K) -
2013Volume 83Issue 1 Pages 158-159
Published: December 14, 2013
Released on J-STAGE: December 21, 2013
Download PDF (349K)