Volume 77, Issue 2
Displaying 1-50 of 57 articles from this issue
-
2010Volume 77Issue 2 Pages 1-14
Published: 2010
Released on J-STAGE: July 25, 2013
Download PDF (4473K)
-
2010Volume 77Issue 2 Pages 31-34
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (1130K) -
2010Volume 77Issue 2 Pages 35-39
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (1034K) -
2010Volume 77Issue 2 Pages 40-43
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (890K) -
2010Volume 77Issue 2 Pages 44-48
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (738K)
-
2010Volume 77Issue 2 Pages 49-52
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (805K)
-
2010Volume 77Issue 2 Pages 54-55
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (749K)
-
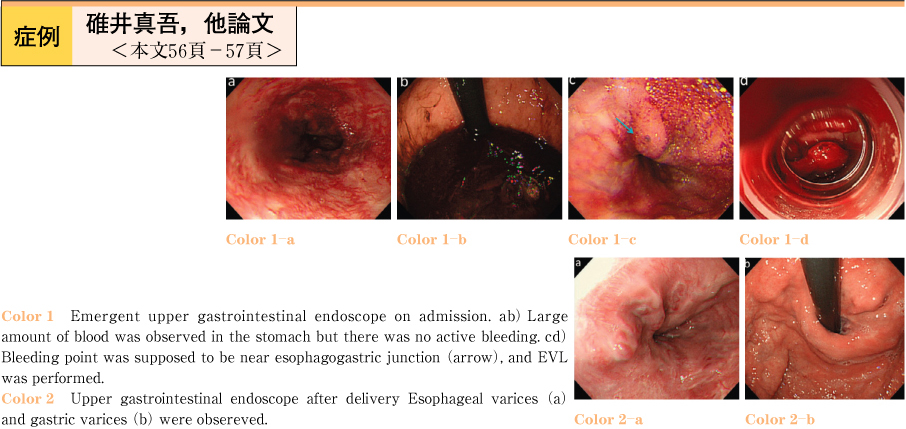
2010Volume 77Issue 2 Pages 56-57
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (736K) -
2010Volume 77Issue 2 Pages 58-59
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (695K) -
2010Volume 77Issue 2 Pages 60-61
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (674K) -
2010Volume 77Issue 2 Pages 62-63
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (998K) -
2010Volume 77Issue 2 Pages 64-65
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (725K) -
2010Volume 77Issue 2 Pages 66-67
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (844K) -
2010Volume 77Issue 2 Pages 68-69
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (712K) -
2010Volume 77Issue 2 Pages 70-71
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (754K) -
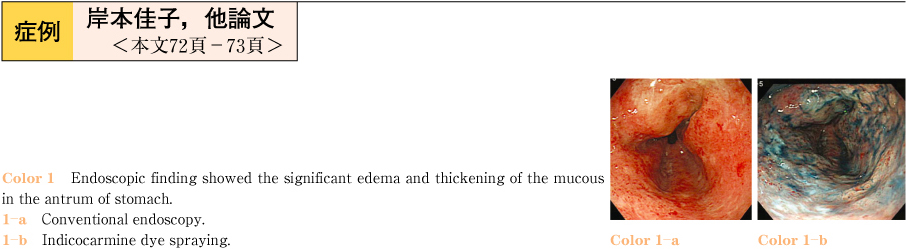
2010Volume 77Issue 2 Pages 72-73
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (850K) -
2010Volume 77Issue 2 Pages 74-75
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (869K) -
2010Volume 77Issue 2 Pages 76-77
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (815K) -
2010Volume 77Issue 2 Pages 78-79
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (687K) -
2010Volume 77Issue 2 Pages 80-81
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (1024K) -
2010Volume 77Issue 2 Pages 82-83
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (775K) -
2010Volume 77Issue 2 Pages 84-85
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (656K) -
2010Volume 77Issue 2 Pages 86-87
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (889K) -
2010Volume 77Issue 2 Pages 88-89
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (792K) -
2010Volume 77Issue 2 Pages 90-91
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (773K) -
2010Volume 77Issue 2 Pages 92-93
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (683K) -
2010Volume 77Issue 2 Pages 94-95
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (909K) -
2010Volume 77Issue 2 Pages 96-97
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (802K) -
2010Volume 77Issue 2 Pages 98-99
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (654K) -
2010Volume 77Issue 2 Pages 100-101
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (761K) -
2010Volume 77Issue 2 Pages 102-103
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (839K) -
2010Volume 77Issue 2 Pages 104-105
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (1018K) -
2010Volume 77Issue 2 Pages 106-107
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (648K) -
2010Volume 77Issue 2 Pages 108-109
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (813K) -
2010Volume 77Issue 2 Pages 110-111
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (851K) -
2010Volume 77Issue 2 Pages 112-113
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (565K) -
2010Volume 77Issue 2 Pages 114-115
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (809K) -
2010Volume 77Issue 2 Pages 116-117
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (807K) -
2010Volume 77Issue 2 Pages 118-119
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (743K) -
2010Volume 77Issue 2 Pages 120-121
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (848K) -
2010Volume 77Issue 2 Pages 122-123
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (760K) -
2010Volume 77Issue 2 Pages 124-125
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (700K) -
2010Volume 77Issue 2 Pages 126-127
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (651K) -
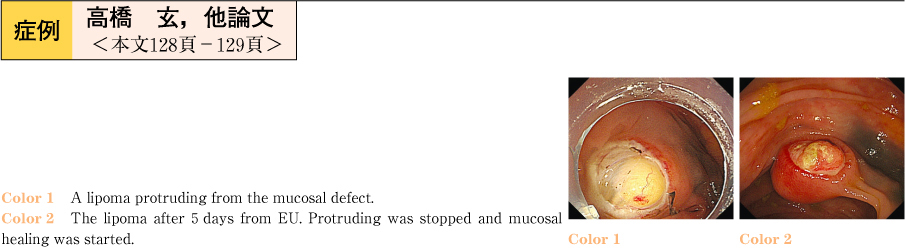
2010Volume 77Issue 2 Pages 128-129
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (740K) -
2010Volume 77Issue 2 Pages 130-131
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (720K) -
2010Volume 77Issue 2 Pages 132-133
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (860K) -
2010Volume 77Issue 2 Pages 134-135
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (742K) -
2010Volume 77Issue 2 Pages 136-137
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (949K) -
2010Volume 77Issue 2 Pages 138-139
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (792K) -
2010Volume 77Issue 2 Pages 140-141
Published: December 10, 2010
Released on J-STAGE: July 25, 2013
Download PDF (821K)