Volume 59, Issue 2
Displaying 1-44 of 44 articles from this issue
- |<
- <
- 1
- >
- >|
-
2001Volume 59Issue 2 Pages 1-9
Published: 2001
Released on J-STAGE: May 22, 2014
Download PDF (8484K)
Technology and instrument
-
2001Volume 59Issue 2 Pages 24-26
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (824K)
Clinical study
-
2001Volume 59Issue 2 Pages 27-31
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (906K) -
2001Volume 59Issue 2 Pages 32-36
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (552K) -
2001Volume 59Issue 2 Pages 37-41
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (2262K) -
2001Volume 59Issue 2 Pages 42-46
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (528K)
Case report
-
2001Volume 59Issue 2 Pages 48-51
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (2170K) -
2001Volume 59Issue 2 Pages 52-55
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (1226K) -
2001Volume 59Issue 2 Pages 56-59
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (1381K) -
2001Volume 59Issue 2 Pages 62-63
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (370K) -
2001Volume 59Issue 2 Pages 64-65
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (840K) -
2001Volume 59Issue 2 Pages 66-67
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (644K) -
2001Volume 59Issue 2 Pages 68-69
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (564K) -
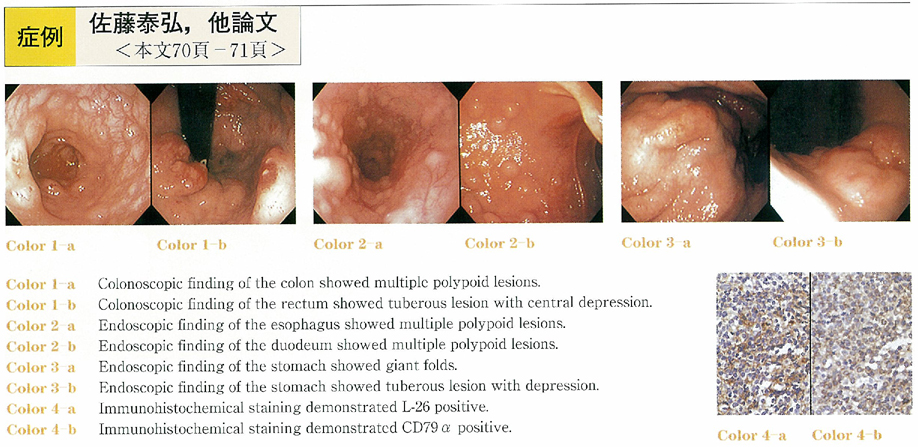
2001Volume 59Issue 2 Pages 70-71
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (936K) -
2001Volume 59Issue 2 Pages 72-73
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (370K) -
2001Volume 59Issue 2 Pages 74-75
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (425K) -
2001Volume 59Issue 2 Pages 76-77
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (909K) -
2001Volume 59Issue 2 Pages 78-79
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (927K) -
2001Volume 59Issue 2 Pages 80-81
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (928K) -
2001Volume 59Issue 2 Pages 82-83
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (810K) -
2001Volume 59Issue 2 Pages 84-85
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (589K) -
2001Volume 59Issue 2 Pages 86-87
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (904K) -
2001Volume 59Issue 2 Pages 88-89
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (1112K) -
2001Volume 59Issue 2 Pages 90-91
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (648K) -
2001Volume 59Issue 2 Pages 92-93
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (461K) -
2001Volume 59Issue 2 Pages 94-95
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (422K) -
2001Volume 59Issue 2 Pages 96-97
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (968K) -
2001Volume 59Issue 2 Pages 98-99
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (914K) -
2001Volume 59Issue 2 Pages 100-101
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (574K) -
2001Volume 59Issue 2 Pages 102-103
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (261K) -
2001Volume 59Issue 2 Pages 104-105
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (983K) -
2001Volume 59Issue 2 Pages 106-107
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (1032K) -
2001Volume 59Issue 2 Pages 108-109
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (266K) -
2001Volume 59Issue 2 Pages 110-111
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (593K) -
2001Volume 59Issue 2 Pages 112-113
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (658K) -
2001Volume 59Issue 2 Pages 114-115
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (672K) -
2001Volume 59Issue 2 Pages 116-117
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (837K) -
2001Volume 59Issue 2 Pages 118-119
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (434K) -
2001Volume 59Issue 2 Pages 120-121
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (226K) -
2001Volume 59Issue 2 Pages 122-123
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (784K) -
2001Volume 59Issue 2 Pages 124-125
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (291K) -
2001Volume 59Issue 2 Pages 126-127
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (566K) -
2001Volume 59Issue 2 Pages 128-129
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (674K) -
2001Volume 59Issue 2 Pages 130-131
Published: December 05, 2001
Released on J-STAGE: May 22, 2014
Download PDF (1232K)
- |<
- <
- 1
- >
- >|