
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Yasuyuki SetoArticle type: FEATURE ARTICLE: 50TH ANNIVERSARY VOLUME
2017Volume 50Issue 5 Pages fa1-
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLDownload PDF (678K) Full view HTML
-
Aya Matsui, Hayato Hosoi, Junkichi Koinuma, Kazuaki Hazama, Kazuhiro I ...Article type: ORIGINAL ARTICLE
2017Volume 50Issue 5 Pages 339-349
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLPurpose: To evaluate the protective benefits of Seprafilm® in reducing adhesive small bowel obstruction after colorectal cancer surgery. Methods: We retrospectively evaluated 583 consecutive patients who underwent open or laparoscopic resection of colorectal cancer. Small bowel obstructions that caused symptoms after evidence of return of bowel function with radiographic confirmation were identified, then patterns and details were analyzed in the Seprafilm® group (n=316) with Seprafilm® applied under the laparotomy wound and the control group (n=267) without Seprafilm®. Findings at re-laparotomy were also investigated in both groups. Results: Postoperative complications, length of hospital stay, and oncological outcomes were comparable in the Seprafilm® group and control group. Morbidity of small bowel obstruction excluding cancer-associated condition was 4.6% (n=27) in the Seprafilm® group and 4.9% (n=29) in the control group (P=0.397). Seven in the Seprafilm® group and 8 in the control group required surgery to relieve obstruction (P=1.000), 2 of which adhesion to the wound were responsible for obstruction in both groups (P=0.625). At re-laparotomy, frequency and severity of adhesion to the previous wound was not significantly different between the two groups. Multivariate analysis of factors including the American Society of Anesthesiologist Performance Status Classification, body mass index, previous abdominal surgery, rectal cancer, length of surgery, blood loss, open surgery, stoma creation, and Seprafilm®, demonstrated that only stoma creation was a significant risk to small bowel obstruction (HR 2.68, 95%CI 1.21–5.96). Conclusions: As small numbers of bowel obstructions were caused by adhesion to the laparotomy wound, our study did not show significant protective benefits of Seprafilm® in reducing small bowel obstruction following colorectal cancer surgery.
View full abstractDownload PDF (1278K) Full view HTML
-
Jongsung Pak, Kazuyoshi Yamamoto, Kazuhiro Nishikawa, Motohiro Hirao, ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 350-356
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLA 73-year-old man had a chief complaint of anorexia and we diagnosed a huge gastric GIST with peritoneal dissemination. Imatinib mesylate (imatinib) (400 mg/day) was given orally and CT revealed a reduction in tumor diameter of 45% a month after start of imatinib therapy. However continuation of imatinib therapy was difficult because of repeated adverse events such as febrile neutropenia and anorexia. He was diagnosed with the abscess formation in the tumor because of the fistulation between the gastric lumen and the tumor by CT and underwent surgery to control infection. The gastric GIST adhered to the transverse colon and the pancreas so he underwent proximal gastrectomy, partial resection of transverse colon, distal pancreatectomy and splenectomy. Peritoneal dissemination was also resected as much as possible. Microscopic findings of resected specimen revealed that there was no viable GIST cells. Forty-five days after the surgery, imatinib (400 mg/day) was resumed and he has been in good health without a recurrence for 18 months after the surgery.
View full abstractDownload PDF (2477K) Full view HTML -
Junko Matsuyama, Manabu Yamamoto, Kenichi Taguchi, Ippei Uezu, Hiroyuk ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 357-363
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
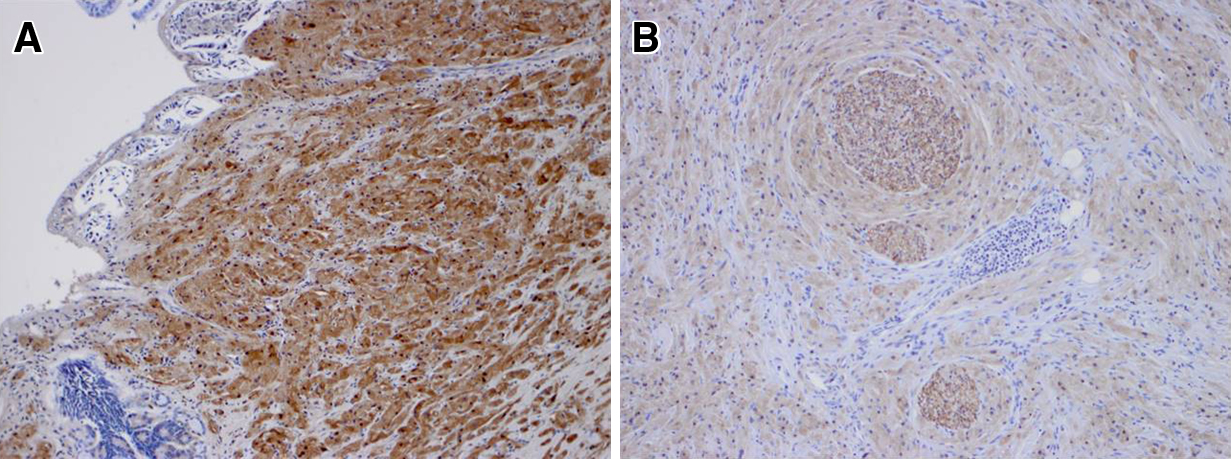
JOURNAL FREE ACCESS FULL-TEXT HTMLWe report a case of a 24-year-old woman with submucosal tumor-like gastric cancer. Before surgery, three malignant lesions were recognized by upper gastrointestinal endoscopy. She had undergone laparoscopic total gastrectomy. We recognized malignant lesions (183 signet-ring cell carcinoma lesions) in the resected specimen after surgery. Her grandmother and father had died of diffuse gastric cancer. She has received S-1 p.o. for 1 year, and has been doing well without any recurrence for 15 months. This case was a clinical hereditary diffuse gastric cancer, though the immunohistochemical staining of E-cadherin on malignant cells was positive.
View full abstractDownload PDF (2225K) Full view HTML -
Takanori Jinno, Yasuhiro Kurumiya, Ei Sekoguchi, Satoshi Kobayashi, Ki ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 364-371
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLA 61-year-old man had undergone curative distal gastrectomy and D2 lymph node dissection for advanced gastric cancer. We administered postoperative chemotherapy with S-1. Twelve months after the operation, an abdominal CT scan showed a marked swelling of the para-aortic lymph node. Seven cycles of S-1+PAC and 6 cycles of S-1+DOC were carried out, but was changed to CPT-11+CDDP because of increased CEA values 9 months after the start of treatment. The CEA value was reduced after the change, the abdominal CT scan revealed that the para-aortic lymph node was smaller. Because PET revealed only a swelling of the para-aortic lymph node, we performed a para-aortic lymph node dissection, and the left renal vein combined resection 2 years from the initial surgery. We used postoperative chemotherapy with 3 cycles of CPT-11+CDDP, and observed. The patient is presently alive with no signs of recurrence after 5 years from the dissection. In para-aortic lymph node metastases of gastric cancer after surgery, because some cases have extended prognosis or are curative by dissection, it is necessary to accumulate and examine further cases related to adaptation and treatment strategy.
View full abstractDownload PDF (1883K) Full view HTML -
Yasunori Uesato, Hiroki Sunagawa, Tadashi NishimakiArticle type: CASE REPORT
2017Volume 50Issue 5 Pages 372-378
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLPancreas preserving total duodenectomy (PPTD) is rarely performed in patients with duodenal disease. In addition, because PPTD was performed in the past by opening the entire abdomen, case reports of laparoscopic-assisted PPTD (LAPPTD) in patients with duodenal disease are rarer still. Here, we report the case of a 64-year-old man with diabetes in whom abnormal duodenal mucosa was found on endoscopy. The lesion was located close to Vater’s papilla, making endoscopic excision difficult; therefore, we planned a surgical duodenectomy. Since imaging findings indicated the lesion to be benign or a non-invasive carcinoma, and the patient had diabetes, we decided to perform PPTD. Additionally, to reduce operative stress, we opted for LAPPTD. Due to excess visceral fat, the surgical time was 11 h 10 min. He had a postoperative course without severe complications, and was followed up for 2 years 6 months, during which he had no relapse or severe complications. We consider this operative method to be admissible in cases of benign or non-invasive duodenal cancer in which pancreas preservation is desirable.
View full abstractDownload PDF (2356K) Full view HTML -
Naoki Mori, Naoki Sakurai, Hajime Iizawa, Shinya OgataArticle type: CASE REPORT
2017Volume 50Issue 5 Pages 379-385
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLA 45-year-old woman, who had been treated for idiopathic thrombocytopenic purpura (ITP), was introduced to surgery because of the difficulty in medical treatment. Splenectomy was performed by hand-assisted laparoscopic surgery (HALS), and she was discharged on postoperative day (POD) 6. On POD 17, CT showed multiple intrahepatic aneurysms. Histopathological examination of the resected specimens showed vacuolar and fibrotic degenerative changes in the main and small artery of the splenic hilum. We thought that multiple intrahepatic aneurysms had been caused by segmental arterial mediolysis (SAM). The aneurysm had disappeared on CT 10 months after observation.
View full abstractDownload PDF (1418K) Full view HTML -
Eiji Hayashi, Yoshito Okada, Yohei Takahashi, Satoko ShimadaArticle type: CASE REPORT
2017Volume 50Issue 5 Pages 386-392
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLWe report a case of granular cell tumor at the hepatic hilum mimicking hilar bile duct carcinoma. The patient was a 38-year-old woman. She was admitted to our hospital for investigation of her liver dysfunction. Enhanced CT and MRI showed a soft mass about 2 cm in diameter at the left hepatic duct with intrahepatic biliary dilatation in the left hepatic lobe. Subsequent imaging with MRCP and ERCP revealed a stricture at the left hepatic duct. Endoscopic biopsy of the stricture revealed atypical cells. Suspicion of cholangiocarcinoma prompted surgery. The patient underwent left hemi-hepatectomy with extrahepatic bile duct excision. The biliary tract was reconstructed with a Roux-en Y choledochojejunostomy. Pathological examination of the specimen revealed a stricture at the left hepatic duct surrounded by a 22-mm mass. The lesion was a benign granular cell tumor. The postoperative course was uneventful, and the patient has been doing well and recurrence free 1 1/2 years after presentation. To the best of our knowledge, this is the first documented case of a granular cell tumor of the hepatic hilum in Japan.
 View full abstractDownload PDF (2153K) Full view HTML
View full abstractDownload PDF (2153K) Full view HTML -
Yuki Higashi, Koichi Shimizu, Toshifumi Watanabe, Shiro Terai, Youhei ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 393-400
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLA 49-year-old woman had undergone CT as a periodic checkup for breast cancer. CT revealed dilatation of the bile duct. She was given a diagnosis of bile duct cancer and gallbladder cancer with pancreaticobiliary maljunction and underwent pylorus-preserving pancreatoduodenectomy. The histopathological diagnosis was adenocarcinoma of the extrahepatic bile duct (T1 N0 M0 Stage I) and gallbladder adenocarcinoma (T1 N0 M0 Stage I). Eighteen months later, CT revealed a hypovascular tumor at the remnant pancreas. The patient was suspected to have remnant pancreatic cancer and underwent total remnant pancreatectomy. Histological sections of the resected specimens showed an irregular arrangement of many white tumors in the remnant pancreas. The uniform atypia of the pancreatic duct exhibited a papillary epithelium. Immunohistochemical analysis showed identical profiles between the remnant pancreatic tumor and the extrahepatic bile duct tumor. Therefore, we diagnosed recurrent bile duct carcinoma at the remnant pancreas. These findings suggest that the extrahepatic bile duct tumor cells disseminated to the pancreatic ducts through the common duct of the pancreaticobiliary maljunction. This is the first known reported case of this condition. Physicians must keep in mind the possibility of dissemination of bile duct carcinoma with pancreaticobiliary maljunction to the remnant pancreas through the common duct.
View full abstractDownload PDF (3468K) Full view HTML -
Shingo Maeda, Norihiro Yuasa, Eiji Takeuchi, Yasutomo Goto, Hideo Miya ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 401-408
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLAn 85-year-old woman visited our hospital with a history of abdominal pain and watery diarrhea. She had not been treated or given antibiotics for any other disease during the 3 months since the onset of the symptoms. Fecal test using rapid enzyme immunoassay showed positive results for glutamate dehydrogenase (GDH) antigen and negative for Clostridium difficile (CD) toxin, on the basis of which we diagnosed infectious enteritis. On the fourth day after admission, she developed severe abdominal pain, and CT revealed abdominal free air. In addition, bacterial culture of the feces obtained on admission revealed CD, and the result of the rapid test using enzyme immunoassay of the CD colony became positive for CD toxin. Thus, a colonic perforation due to CD colitis was diagnosed, following which an emergency surgery was performed. Laparotomy revealed perforations in the sigmoid colon and deteriorated color of the descending and sigmoid colon; therefore, left hemicolectomy and transverse colostomy were performed. Fulminant CD colitis can occur in the absence of history of treatment for any other disease or prior administration of antibiotics. Treatment of CD colitis should be initiated when investigations yield positive results for fecal GDH antigen and when CD colitis is suspected according to the clinical presentation.
View full abstractDownload PDF (2429K) Full view HTML -
Ryuta Muraki, Masayoshi Yamamoto, Shintaro Ishikawa, Takahumi Kawamura ...Article type: CASE REPORT
2017Volume 50Issue 5 Pages 409-415
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLA 57-year-old woman was seen at a local medical doctor for a discomfort of defecation. Colonoscopy was performed at the hospital and submucosal tumor was found in the Rb rectum. Endoscopic submucosal resection was performed and the resected specimen was histologically diagnosed as neuroendocrine tumor (NET; G1). She was admitted to our hospital for additional radical resection. CT and MRI showed swollen left lateral pelvic lymph nodes that were suspected as lymph nodes metastases. Laparoscopic super low anterior resection with left-side lateral pelvic lymph node dissection was performed. Resected lymph nodes were histologically diagnosed as metastases of NET. In this paper, we reviewed reported 4 cases of lateral pelvic lymph node metastasis of NET. Pre-operative CT or MRI examination is indispensable for the detection of lateral pelvic lymph node metastasis regardless of tumor size or macroscopic morphology. In cases of NET with lateral pelvic lymph node metastasis, better clinical outcome could be achieved by radical lateral lymph node dissection according to the treatment for rectal cancer.
View full abstractDownload PDF (2211K) Full view HTML
-
Takako Kojima, J. Patrick BarronArticle type: SPECIAL CONTRIBUTION
2017Volume 50Issue 5 Pages 416-417
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLDownload PDF (987K) Full view HTML
-
Ichiro UyamaArticle type: EDITOR'S NOTE
2017Volume 50Issue 5 Pages en5-
Published: May 01, 2017
Released on J-STAGE: May 25, 2017
JOURNAL FREE ACCESS FULL-TEXT HTMLDownload PDF (679K) Full view HTML
- |<
- <
- 1
- >
- >|