
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Kyohei Ogawa, Ryota Higuchi, Takehisa Yazawa, Shuichiro Uemura, Wataru ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 675-683
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLDistal bile duct metastasis of colorectal cancer is a rare presentation. The patient was an 82-year-old man who had previously undergone ileocecal resection, partial resection of the stomach, and left hepatectomy for ascending colon cancer, early gastric cancer, and liver metastasis of the colon cancer, respectively, when he was 80 years old. The patient received adjuvant combination chemotherapy of S-1 and oxaliplatin plus bevacizumab. Two years later, during routine follow up, CT scans revealed a high-density tumor with a diameter of 22 mm in the distal bile duct. ERCP also revealed a defect in the distal bile duct, and subsequent biopsy confirmed that the tumor was an adenocarcinoma. Pylorus-preserving pancreaticoduodenectomy (PPPD) was performed based on the diagnosis of distal cholangiocarcinoma. A 35-mm papillary tumor was found in the resected specimen. Pathologically, the tumor was a moderately differentiated tubular adenocarcinoma. The morphology and immunohistochemical staining patterns of the tumor cells were similar to those of the previous colon cancer. Thus, the tumor was strongly suspected to be a bile duct metastasis of the colon cancer. The patient’s recovery following surgery was unremarkable and there has been no recurrence to date.
 View full abstractDownload PDF (1832K) Full view HTML
View full abstractDownload PDF (1832K) Full view HTML -
Masahiro Yamamoto, Noboru Ideno, Toshiya Abe, Naoki Ikenaga, Kohei Nak ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 684-691
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe experienced a case of worsening of celiac artery (CA) stenosis after pancreaticoduodenectomy (PD) that was treated by urgent median arcuate ligament release (MALR), despite this procedure being judged unnecessary preoperatively and intraoperatively. A 64-year-old woman was found to have stenosis at the root of the CA, but no development of collateral circulation via the gastroduodenal artery (GDA) on a preoperative CT scan. An intraoperative GDA clamp test revealed no sign of decreased hepatic artery blood flow. Hence, we judged MALR not to be necessary at that time. However, on postoperative day 1, hepatopancreatic enzymes elevated markedly and a contrast CT scan revealed worsening of CA stenosis. This resulted in ischemia in the left lateral segment of the liver, stomach, remnant pancreas and spleen. Urgent MALR was performed, and immediate improvement of hepatic artery blood flow and alleviation of organ ischemia was confirmed. This case suggests that worsening of CA stenosis may occur due to postoperative changes in hemodynamics or respiratory condition, or edematous changes in retroperitoneal tissues, even if MALR is initially judged to be unnecessary in PD cases with CA stenosis.
 View full abstractDownload PDF (961K) Full view HTML
View full abstractDownload PDF (961K) Full view HTML -
Yui Hoshino, Masayuki Tsutsuyama, Hiroyuki Sugimoto, Daisuke Kobayashi ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 692-700
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLAn 85-year-old man was referred to our hospital due to frequent vomiting and abdominal pain. Abdominal CT revealed a jejunum tumor and small bowel obstruction. Laboratory tests showed elevated CA19-9 of 601.3 U/ml. Conservative treatment failed to improve the symptoms. Laparotomy identified an obstruction of the jejunum about 70 cm distal from Treitz’s ligament. Small bowel partial resection was performed, including the 5-cm tumor and dissected lymph nodes. Pathological examination revealed adenocarcinoma arising from a Heinrich type II aberrant pancreatic tumor in the jejunum. Radical resection was possible; however, two months after surgery, multiple liver metastases and intra-abdominal lymph node recurrence were found. The patient has since been treated with S-1. Aberrant pancreatic cancer in the small intestine is rare and difficult to diagnose preoperatively. We report this case with a review of the literature.
View full abstractDownload PDF (1535K) Full view HTML -
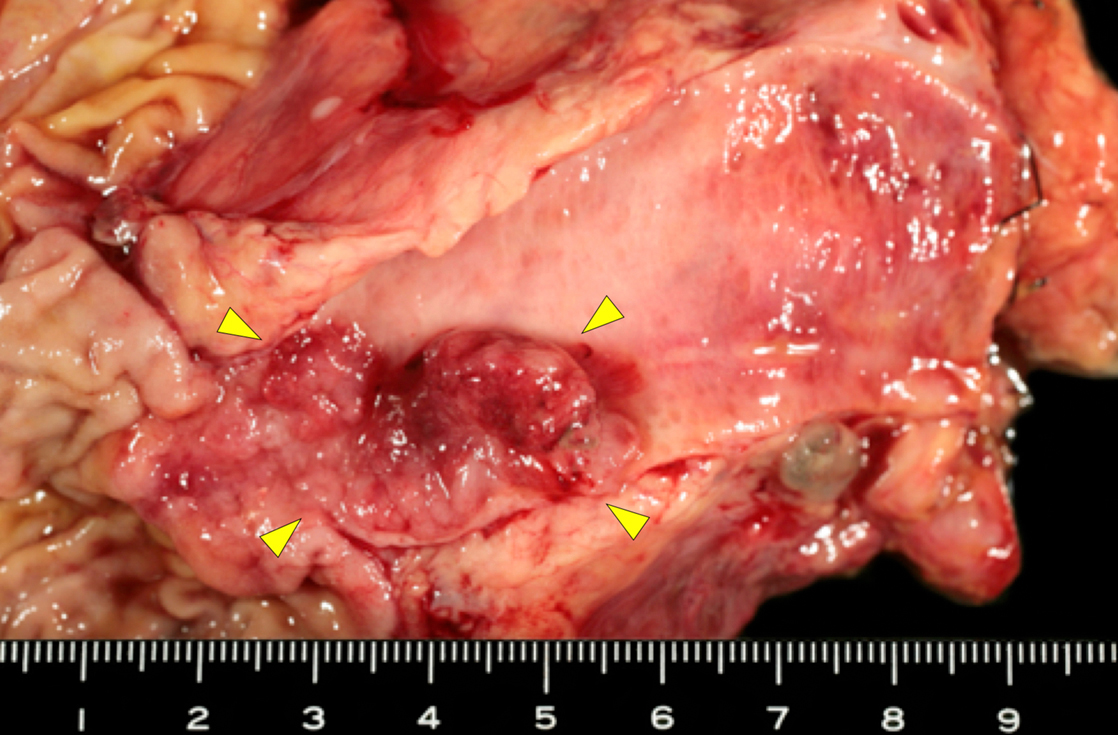
Daisuke Hara, Kengo Kai, Takuto Ikeda, Akiko Ichihara, Mayu Inomata, S ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 701-708
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 74-year-old man presented to the dermatology department of our hospital with multiple eruptions with itching. Leser-Trélat was suspected due to a rapid increase in seborrheic keratosis. Colonoscopy revealed a 35-mm multinodular polypoid lesion with a laterally spreading tumor that was partially non-granular. The tumor was diagnosed as carcinoma in adenoma with submucosal invasion. Because of the difficulty of endoscopic en bloc resection, laparoscopic ileocecal resection was performed in our department. A pathologic examination revealed that the resected cancer was a minute carcinoma in situ, of only 500 μm in size. We confirmed that the skin lesions were related to the Leser-Trélat sign, based on improvement of the skin after resection of colon cancer and high expression of epidermal growth factor receptor in the skin lesions. The Leser-Trélat sign, a skin symptom of paraneoplastic dermadromes, is frequently associated with gastrointestinal cancers, such as gastric and colorectal cancer, and is reported to be associated with advanced stage disease. In contrast, reports of the sign in association with early colorectal cancer are rare. Our search of the Japanese literature yielded only 3 cases in which the sign was described in submucosal invasive cancer and none involving intramucosal cancer. We present this case of minute carcinoma in situ in the ascending colon with a Leser-Trélat sign and review the relevant literature to investigate the clinical differences between cases of early and advanced cancer with a Leser-Trélat sign.
 View full abstractDownload PDF (1351K) Full view HTML
View full abstractDownload PDF (1351K) Full view HTML -
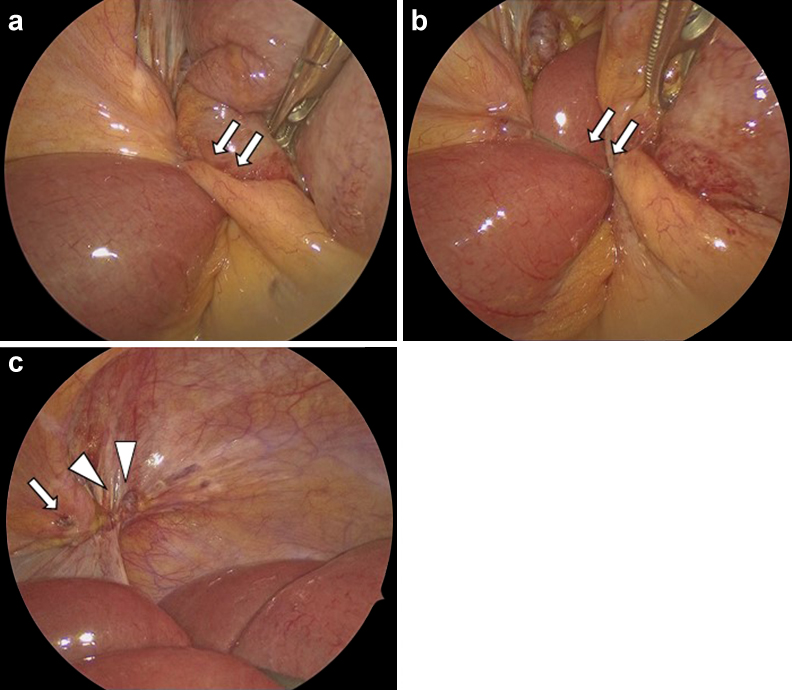
Yasunori Yoshimoto, Satoshi Taniwaki, Tomohisa Shimokobe, Tetsuo Imamu ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 709-717
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 42-year-old woman underwent transanal total mesorectal excision (TaTME) with a covering ileostomy for rectal cancer (Rb). She was discharged 16 days after surgery without any major problems. Since the cancer was pT2N1aM0 Stage IIIa, the covering ileostomy was closed after postoperative adjuvant chemotherapy. One week after discharge, a rectovaginal fistula became apparent. The patient was administered estriol tablets alone, which resulted in the rectovaginal fistula healing after approximately 2 months. Rectovaginal fistula is usually difficult to relieve with conservative treatment alone, and invasive treatment is often required. However, in recent years, reports of improvement with estriol administration have suggested that this may be a minimally invasive and effective conservative treatment for postoperative rectovaginal fistula.
 View full abstractDownload PDF (1370K) Full view HTML
View full abstractDownload PDF (1370K) Full view HTML -
Takashi Sakuma, Hitoshi Teraoka, Taichi Shoji, Haruhito Kinoshita, Yas ...Article type: CASE REPORT
2022Volume 55Issue 11 Pages 718-724
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLAn 80-year-old male underwent laparoscopic hernia repair for bilateral internal inguinal hernia. He was discharged on postoperative day (POD) 1; however, on POD 8, he returned to our department with chief complaints of abdominal distension, abdominal pain, and vomiting. He was diagnosed with adhesive intestinal obstruction, but the obstruction did not resolve with conservative management with an ileus tube. He finally underwent laparoscopic reoperation for the obstruction on POD 13. During this procedure, the end of the barbed suture used for peritoneum closure in the hernia repair was found to have migrated into the nearby mesentery of the small bowel and formed a band that directly compressed the terminal ileum and caused small intestinal obstruction. The obstruction was released by cutting and pulling out the free edge of the barbed suture. Neither intestinal resection nor peritoneum reclosure was needed. The patient was discharged on re-POD 5 without any complications. The use of barbed suture is convenient and time-saving, and is used in various surgical departments. However, our case suggests that there is a risk of intestinal obstruction or intestinal volvulus due to barbed suture. Avoiding exposure of the free edge of the barbed suture in the peritoneal cavity, such as cutting the free edge as short as possible or using a non-barbed suture above the barbed suture, might contribute to reduction of these complications.
 View full abstractDownload PDF (770K) Full view HTML
View full abstractDownload PDF (770K) Full view HTML
-
Masaya Uesato, Yukiya Sato, Manami Kobayashi, Shohei Yonemoto, Yuichir ...Article type: PRELIMINARY REPORTS
2022Volume 55Issue 11 Pages 725-728
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTML
-
[in Japanese], [in Japanese], [in Japanese], [in Japanese], [in Japane ...Article type: SPECIAL REPORT
2022Volume 55Issue 11 Pages 729-732
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTML
-
Takeshi KubotaArticle type: EDITOR'S NOTE
2022Volume 55Issue 11 Pages en11-
Published: November 01, 2022
Released on J-STAGE: November 30, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLDownload PDF (196K) Full view HTML
- |<
- <
- 1
- >
- >|
