
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Kaichiro Harada, Kenya Yamanaka, Makoto Kurimoto, Masashi Kayano, Misa ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 233-239
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLThere are few reports of hemorrhagic rupture of liver cysts. Here, we report a case of emergency surgery for hemorrhagic shock due to a ruptured hepatic cyst in a 91-year-old woman. The patient was treated under a diagnosis of pyelonephritis and septic shock at another hospital. She had acute lower right abdominal pain and her vital signs were in pre-shock, and she was transferred to our hospital. Contrast-enhanced CT showed a cystic lesion in the posterior segment of the liver and ascites with a high CT value around the liver. She was diagnosed with hemorrhagic shock due to hemorrhagic rupture of a liver cyst. The CT examination revealed no extravasation. Thus, transcatheter hemostasis was thought to be inapplicable, and emergency surgery for hemostasis was selected. The right lobe of the liver was mobilized under the Pringle maneuver to expose the wall of the hepatic cyst. Bleeding from the ruptured hepatic cyst was confirmed and hemorrhagic rupture of the liver cyst was diagnosed intraoperatively. The cyst wall was excised to identify and suture the bleeding site in the Glissonean sheath. The ascites in the Douglas fossa was infectious. We concluded that hepatic cyst bleeding triggered by hepatic cyst infection and subsequent cyst rupture led to hemorrhagic shock with acute abdominal pain. Despite her advanced age of 91 years old, the patient was discharged after 14 days without surgical complications.
 View full abstractDownload PDF (1038K) Full view HTML
View full abstractDownload PDF (1038K) Full view HTML -
Takayuki Minami, Takashi Mizuno, Junpei Yamaguchi, Shunsuke Onoe, Nobu ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 240-250
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe report two cases of cholangiocarcinoma with a small cell carcinoma (SCC) component that exhibited contrasting courses after resection, with early death versus long-term survival. Case 1 was a 70-year-old man who underwent left hepatectomy with caudate lobectomy for perihilar cholangiocarcinoma. Histopathological examination showed adeno-neuroendocrine carcinoma composed of papillary adenocarcinoma and SCC. The tumor was classified as pT2N0M0, Stage II, but with extensive venous invasion from SCC. Gemcitabine alone was administered postoperatively based on normal treatment of biliary tract cancer, but the patient died only five months after surgery due to early relapse with multiple liver metastases. Case 2 was a 65-year-old man who underwent subtotal stomach preserving pancreatoduodenectomy for distal cholangiocarcinoma. Histopathological examination showed neuroendocrine SCC with lymph node metastasis. The tumor was classified as pT2N1M0, Stage III. As standard chemotherapy for pulmonary SCC, cisplatin plus etoposide was given for 4 cycles postoperatively. The patient has been alive without recurrence for 8 years after surgery. An SCC component in cholangiocarcinoma often leads to early relapse with subsequent cancer-related death after resection. Therefore, multidisciplinary approach including chemotherapy similar to that for pulmonary SCC should be considered in this setting.
 View full abstractDownload PDF (2127K) Full view HTML
View full abstractDownload PDF (2127K) Full view HTML -
Miyuki Atarashi, Shunji Kawamoto, Kota Yamamoto, Takahiro TerashimaArticle type: CASE REPORT
2022Volume 55Issue 4 Pages 251-259
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 56-year-old woman who was a Jehovah’s Witnesses was diagnosed with advanced gastric cancer (cT3, N0, M0) and a pancreatic cystic tumor. Preoperative abdominal CT indicated an extrahepatic portal vein aneurysm with a diameter of 22 mm. Total gastrectomy plus distal pancreatectomy with splenectomy were performed. Epigastric pain occurred on postoperative day 11. CT revealed a massive portal vein thrombus from the level of the superior mesenteric vein to the bifurcation of the hepatic hilum. Thrombectomy was performed under laparotomy, and thereafter urokinase was administered by intermittent infusion through a catheter placed in a branch of the superior mesenteric vein. The day after the reoperation, abdominal CT revealed massive ascites with a high level of amylase and the thrombosed portal vein aneurysm compressing the body of the pancreas, resulting in development of acute pancreatitis and a pancreatic fistula. Continuous abdominal irrigation followed by a pancreatic duct stent indwelled via the papilla of Vater was associated with improvement of pancreatitis and pancreatic fistula. The portal vein thrombus was gradually reduced in size by a use of warfarin. We report this case as a rare example of a portal vein aneurysm that developed into a postoperative portal vein thrombus and compressed the body of the pancreas, causing pancreatitis and pancreatic fistula at the stump.
View full abstractDownload PDF (812K) Full view HTML -
Shunya Tahara, Takeshi Sudo, Naoto Hadano, Hiroshi Morimoto, Norimitsu ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 260-268
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe report two cases of refractory ascites after surgery for pancreatic cancer that were treated with a Denver shunt®. Case 1 was a 74-year-old man who developed refractory chylous ascites 2 months after subtotal stomach-preserving total pancreatectomy. A Denver Shunt® was placed 6 months after the operation. Case 2 was a 71-year-old woman with a history of liver cirrhosis. Refractory ascites appeared 1 month after pylorus-preserving pancreaticoduodenectomy, and a Denver shunt® was placed 2 months after the operation. It was possible to resume and complete postoperative adjuvant chemotherapy in Case 1 and to start this chemotherapy in Case 2. Ascites was well controlled at 1 year and 10 months after placement of the Denver Shunt® in Case 1 and at 5 months in Case 2. The Denver Shunt® may have the potential to improve the prognosis of patients with non-malignant refractory ascites in the acute postoperative phase after surgery for pancreatic cancer by enabling early control of ascites and permitting introduction and continuation of adjuvant chemotherapy.
 View full abstractDownload PDF (1167K) Full view HTML
View full abstractDownload PDF (1167K) Full view HTML -
Daisuke Taguchi, Yujiro Tsuda, Masahiro Koh, Masami Ueda, Shinsuke Nak ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 269-275
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLThe patient was a 78-year-old woman who had experienced duodenal obstruction fifteen times in the last 5 years. She visited our hospital with complaints of abdominal pain and vomiting. Abdominal CT showed duodenal obstruction and an abnormal position of the duodenum due to reverse intestinal malrotation. She was immediately hospitalized and conservative therapy succeeded in resolving the intestinal obstruction. However, the frequency of duodenal obstruction increased and she requested surgery to prevent recurrence of the symptom. Therefore, we decided to perform an operation during a period of hospitalization. Intraoperative findings indicated that the cause of duodenal obstruction was distortion of the mesentery caused by reverse intestinal malrotation that compressed the duodenal jejunum. The tissue surrounding the duodenal jejunum was exfoliated to allow mobilization and the abnormal position of the duodenum was shifted to normal. The patient was discharged without complications several days after the operation. She has been followed up as an outpatient and has had a good postoperative course without recurrence for more than one year. Reverse intestinal malrotation is a rare congenital anomaly. Our case was the type in which the duodenum rotates in reverse, while the colon rotates normally. We report this case as an example of a good prognosis after surgery for prevention of recurrence of duodenal obstruction in a patient with reverse intestinal malrotation.
View full abstractDownload PDF (1042K) Full view HTML -
Hironori Fujieda, Ryuzo Yamaguchi, Shinya Watanabe, Keiji Aizu, Shinic ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 276-281
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 7-year-old female presented with a chief complaint of right lower quadrant pain. Contrast-enhanced CT revealed swelling of the appendix, with continuous fluid accumulation at the distal appendix. Based on an abscess formation, the patient was suspected to have acute appendicitis. Appendectomy was performed, but the laparotomic findings did not include an abscess. The appendix had swollen in a cystoid manner and was excised, and the condition was found to be gangrenous appendicitis. Circumferential wall thickening was observed in a region 1 cm distal to the appendectomy site, and the distal portion had expanded in a cystoid manner due to an obstruction. Histopathological examination detected an infiltrating tumor reaching the subserous layer of the site of wall thickening of the appendix, with small and relatively evenly sized cells forming a rosette-like structure and a funicular sequence. Immunostaining was strongly positive for chromogranin A, synaptophysin, and CD56, and slightly positive for Ki-67, while D2-40 and CD31 showed infiltration in lymphatic vessels and veins. Thus, the patient was diagnosed with neuroendocrine tumor G2. Given the vascular infiltration, ileocecal resection and D3 lymph node dissection were performed. The patient showed good progress, with no recurrence for 2 years postoperatively.
View full abstractDownload PDF (1119K) Full view HTML -
Sodai Arai, Takatoshi Matsuyama, Akitoshi Nankaku, Masako Mizoguchi, M ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 282-289
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
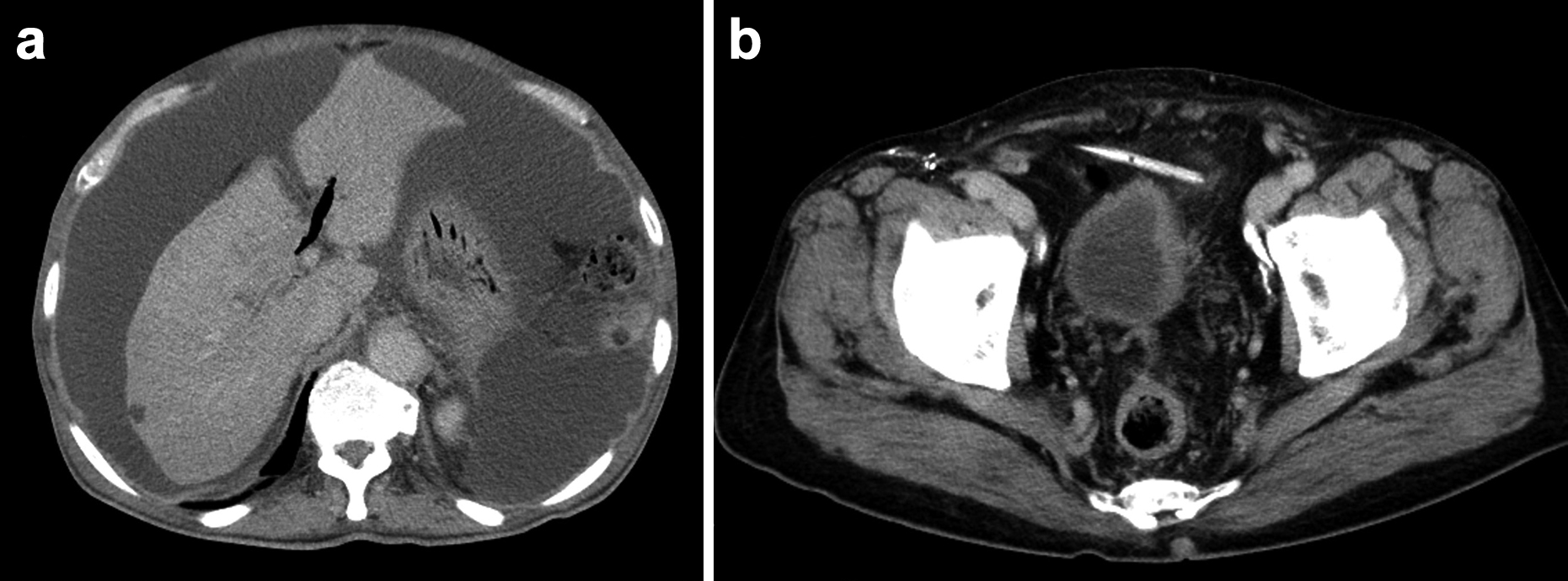
JOURNAL OPEN ACCESS FULL-TEXT HTMLVenous thromboembolism (VTE) is an extraintestinal complication of ulcerative colitis (UC), and such complications lead to a poor prognosis of UC. The most common site of VTE is a deep vein in the leg, whereas VTE rarely occurs in the renal vein. In such cases, placement of a preoperative inferior vena cava filter for renal blood flow protection is difficult, resulting in a high perioperative risk for pulmonary embolism. Our surgical treatment for UC with severe complications is based on a three-stage operation, in which the first stage is subtotal colectomy with end ileostomy. We also usually select laparoscopic surgery to minimize invasion as much as possible. Herein, we report two cases of UC with left renal vein thrombosis preoperatively. The first case was a 26-year-old man with UC refractory to medical therapy, and the second case was a 57-year-old man with UC-associated sigmoid colon cancer. In both cases, we performed laparoscopic subtotal colectomy with end ileostomy, followed by starting antithrombotic drugs immediately after surgery. In both cases, there were no postoperative VTE-related complications.
View full abstractDownload PDF (1050K) Full view HTML -
Kenji Okuda, Yoshito Okada, Shusaku Ohira, Yasuro Taguchi, Yayoi Sakat ...Article type: CASE REPORT
2022Volume 55Issue 4 Pages 290-296
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 79-year-old man visited our hospital due to melena. He had undergone low anterior resection for rectal cancer ten years ago. Abdominal contrast-enhanced CT revealed arteriovenous malformation (AVM) in the pelvis. Colonoscopy showed bleeding at the previous anastomotic site. Interventional radiology (IVR) was performed for treatment. Angiography of the right common iliac artery revealed AVM of the internal iliac artery region. Embolization of the main feeding artery was performed. After the procedure, melena stopped and the patient was discharged, but was then readmitted due to re-bleeding on the next day. Transanal suture of the bleeding site was performed. Based on a tentative conclusion that the bleeding had stopped, the patient was transferred to an IVR specialty facility for curative treatment of AVM. Hemostasis was obtained by embolizing multiple inflow arteries and outflow veins. There has been no recurrence for two years after treatment.
View full abstractDownload PDF (786K) Full view HTML
-
Soichiro IshiharaArticle type: EDITOR'S NOTE
2022Volume 55Issue 4 Pages en4-
Published: April 01, 2022
Released on J-STAGE: April 28, 2022
JOURNAL OPEN ACCESS FULL-TEXT HTMLDownload PDF (173K) Full view HTML
- |<
- <
- 1
- >
- >|