
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Sho Tazuma, Yoichi Sugiyama, Kensuke Shimbara, Kenta Baba, Tatsuya Taz ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 83-90
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 53-year-old man was admitted to our hospital for evaluation of fever and left back pain. Blood tests showed increases in the WBC count and CRP level. Abdominal CT showed liver abscesses, one of which connected the gastric wall of the abscess to the wall of the mid-gastric body. The patient was admitted for treatment with antibiotics and a PPI. The WBC count and CRP level decreased concurrently with a reduction in the size of the liver abscesses. Serial blood cultures were negative for bacterial growth. Upper gastrointestinal endoscopy showed A2 stage ulceration involving the anterior wall in the stomach. Histologic examination of a biopsy specimen revealed moderately differentiated adenocarcinoma. The diagnosis was advanced gastric cancer. During surgery, the tumor was found to have directly invaded the liver and left diaphragm. Total gastrectomy and combined left lateral segmentectomy and resection of the diaphragm were performed. The postoperative course was uneventful and the patient was discharged on postoperative day 15. The pathologic findings revealed gastric cancer (MU, Less-Ant-Post, Type 3, por>sig, pT4b [SI], pN2, pM1 [LYM], pStage IV). Cancer cells and a bacterial mass were present on the fundus of the ulcer. Gram-staining detected branched gram-positive rods similar to Actinomyces species. We speculate in this case that liver abscesses were formed by infection of resident bacteria through the portal vein. Fifty-two months after surgery, the patient is well with no evidence of recurrent diseases.
View full abstractDownload PDF (1172K) Full view HTML -
Yuta Matsuo, Yasuhiro Yuasa, Mizuki Fukuta, Hidenori Maki, Taihei Take ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 91-97
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLThe patient was a 36-year-old man with chief complaints of melena and syncope. He had anemia and decreased blood pressure, and underwent emergency upper gastrointestinal endoscopy. A hemorrhagic varix was found in the descending part of the duodenum. It was difficult to stop bleeding by endoscopy and balloon-occluded retrograde transvenous obliteration (B-RTO); therefore, laparotomy was performed in a hybrid operating room. The varix was ligated together with the duodenal wall, and no blood transfer to the varicose vein was confirmed by intraoperative endoscopy and interventional radiology. This case is a rare example of an isolated duodenal varix with no underlying disease such as liver cirrhosis or findings suggestive of portal hypertension. Endoscopy and interventional radiology are the first-line treatments for varices, but surgery is indicated in cases with difficulty with hemostasis, and performance of this surgery in a hybrid operating room may be useful.
View full abstractDownload PDF (1221K) Full view HTML -
Aya Noguchi, Hiroshi Yoshida, Shinya Kawaguchi, Akihiko Hashimoto, Sat ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 98-106
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 62-year-old woman was referred to our department for further examination and treatment of 24-mm and 22-mm hypoechoic masses of the liver (S4), which were found without symptoms by US. These tumors in contrast-enhanced CT showed weak enhancement in the arterial phase and slight hypodensity compared with surrounding normal liver in the delayed phase. Furthermore, CT during arterial portography and MRI newly revealed an 8-mm tumor in the S1 segment. The tumors were diagnosed as multiple hepatocellular carcinomas and hepatectomy was performed. Left medial sectionectomy was performed because the tumor in S1 was not detected during surgery. The pathological diagnosis was mucosa-associated lymphoid tissue (MALT) lymphoma. The remaining tumor in S1 disappeared after six courses of postoperative rituximab therapy. The patient is alive without recurrence at 3 years and 9 months after hepatectomy. Primary hepatic MALT lymphoma is uncommon and a standard therapy has not been established. Surgical treatment is most common, whereas there are few previous reports of cases treated with multimodal therapy. The clinical course of our case suggests that postoperative rituximab might be effective for residual lesions of hepatic MALT lymphoma.
View full abstractDownload PDF (1156K) Full view HTML -
Ayumi Kanazawa, Yasutoshi Kimura, Masafumi Imamura, Minoru Nagayama, H ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 107-117
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe report a case of hilar cholangiocarcinoma with a complete pathological response following neoadjuvant chemotherapy (NAC) for synchronous gastric cancer. A 36-year-old man was diagnosed with perihilar cholangiocarcinoma (Bismuth type IV, cT3N1M0, cStage IIIB) and gastric cancer (U, cT3N1M0, cStage IIB). Percutaneous transhepatic portal vein embolization (PTPE) was performed because the future liver remnant was too small. During the waiting period, systemic chemotherapy (modified DCS) was administered as NAC for the gastric cancer. The patient underwent right hepatic trisectionectomy combined with bile duct resection, regional lymph node dissection, and total gastrectomy as one-stage radical surgery 210 days after PTPE. The histopathological diagnoses were bile duct cancer (ypT0N0M0, stage 0, pretreatment effect grade 3) and gastric cancer (ypT3N1M0, stage IIB, pretreatment effect grade 2). Postoperatively, adjuvant chemotherapy for gastric cancer was administered with S-1 (tegafur, gimeracil, oteracil potassium) and the patient has survived without recurrence for 34 months since surgery.
 View full abstractDownload PDF (1738K) Full view HTML
View full abstractDownload PDF (1738K) Full view HTML -
Tatsuki Kusuhara, Takashi Ito, Hiroki Matsuoka, Takamasa OhnishiArticle type: CASE REPORT
2021Volume 54Issue 2 Pages 118-124
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe present the case of a 69-year-old woman with an 18-mm mass revealed at the fundus of the gallbladder on abdominal US and an elevated lesion at the same site that was prematurely stained on contrast-enhanced CT. Based on suspected gallbladder carcinoma, laparoscopic cholecystectomy was performed. A mass consisting of solid and cystic components was found on the surface of the fundus of the excised gallbladder, and an intraoperative diagnosis of adenocarcinoma was made using frozen sections. Gallbladder bed resection and lymph node dissection were performed. Most of the tumor was in a dilated cyst, and the cystic epithelium had developed in a papillary and inverted manner. Moreover, infiltration into the subserosa was observed at the fundus of the solid component. The histological diagnosis was intracholecystic papillary neoplasm (ICPN) with an associated invasive carcinoma. The cyst was presumed to have originated from the Rokitansky-Aschoff sinus (RAS), which had filled with tumor-producing mucus that had expanded. An ICPN originating and progressing from the RAS is rare. We describe the case and a review of literature cases.
View full abstractDownload PDF (1584K) Full view HTML -
Yo Hattori, Yoshiro Matsuba, Toshitaka Mamiya, Yoshito Iida, Mitsuhiro ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 125-132
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLIn pancreaticoduodenectomy for a patient with celiac axis (CA) occlusion, cutting off the collateral pathways may lead to ischemia of organs originally supplied by the CA. A 72-year-old man was diagnosed with cancer of the ampulla of Vater upon examination for jaundice. Contrast-enhanced CT showed focal occlusion of the proximal CA with a “hooked appearance” and development of an anomalous arterial arcade of the pancreatic head. The case was complicated by CA occlusion due to compression by the median arcuate ligament (MAL). Surgery was performed with subtotal stomach-preserving pancreaticoduodenectomy, and intraoperative blood flow was evaluated using Doppler US. Clamping of the gastroduodenal artery interrupted blood flow in the common hepatic artery (CHA), so an incision was made in the MAL. However, we could not restore blood flow in the CHA, and thus, resection that preserves the collateral circulation from the superior mesenteric artery via the anterior inferior and superior pancreaticoduodenal arteries was performed. The patient has made satisfactory progress without ischemic events and has survived without recurrence for 2 years at the time of writing. This case shows that collateral circulation-preserving pancreatoduodenectomy for patients with CA occlusion can be safely performed with careful case selection and can be considered as an alternative to revascularization procedures.
 View full abstractDownload PDF (1571K) Full view HTML
View full abstractDownload PDF (1571K) Full view HTML -
Kento Hirotaka, Yasuhisa Mori, Takao Ohtsuka, Yusuke Watanabe, Naoki I ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 133-140
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLWe herein present the case of a 45-year-old asymptomatic female who was referred to our institution for main pancreatic duct stenosis revealed by US. CT and MRI confirmed a well-defined hypervascular tumor of 4 mm in diameter in the head of the pancreas. Endoscopic ultrasound-guided fine needle aspiration and pancreatic juice cytology under ERCP showed no malignancy. Laparoscopy-assisted pancreatoduodenectomy was performed under a preoperative diagnosis of a serotonin-producing pancreatic neuroendocrine tumor (PanNET). Pathological examination of the resected specimen showed that the tumor was a serotonin-producing PanNET.
View full abstractDownload PDF (1306K) Full view HTML -
Tetsuya Murasawa, Maeng Bong Jin, Hiroaki Tottori, Motonori Futatsugi, ...Article type: CASE REPORT
2021Volume 54Issue 2 Pages 141-148
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
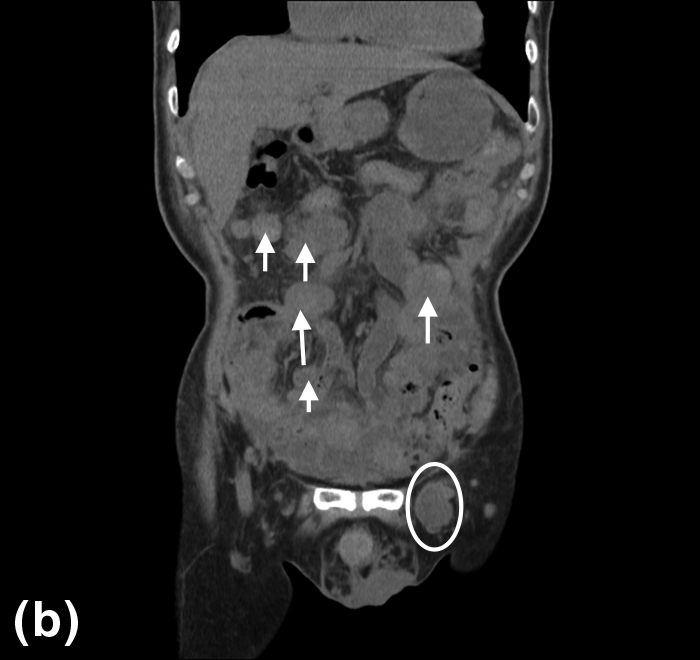
JOURNAL OPEN ACCESS FULL-TEXT HTMLAn 83-year-old man was admitted to our hospital with abdominal pain and swelling around his left groin. A physical examination and contrast-enhanced CT showed an incarcerated femoral hernia and multiple intraabdominal tumors. Emergency surgery was performed and this revealed that the small intestine was incarcerated in the left inguinal ligament, along with an oval-shaped tumor. The hernia was repaired and the tumor was resected. Histology and immunostaining revealed a biphasic malignant peritoneal mesothelioma (MPM). Although the patient was discharged in good condition on postoperative day 8, he returned to hospital with bowel obstruction on day 16 and died on day 26. Malignant mesothelioma is a rare disease arising from mesothelial cells covering the body cavities. It can develop from the pleura, peritoneum, pericardium, and tunica vaginalis of the testis. MPM accounts for 10–20% of all mesotheliomas and is difficult to diagnose because it usually presents with non-specific symptoms. In this case, we report a case of MPM that was diagnosed incidentally with an incarcerated left femoral hernia.
 View full abstractDownload PDF (1350K) Full view HTML
View full abstractDownload PDF (1350K) Full view HTML
-
Yasunao Ishiguro, Masanori Hakozaki, Naruaki Takahashi, Hajime Sato, N ...Article type: CLINICAL EXPERIENCE
2021Volume 54Issue 2 Pages 149-155
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLAdvanced gastric cancer with bleeding may be resected to achieve hemostasis. However, sometimes a case is not suitable for resection because of severe local invasion or a poor condition of the patient. Between April 2013 and March 2018, 21 cases of advanced gastric cancer with anemia (hemoglobin level <10 mg/dl) were treated by radiotherapy for hemostasis at our hospital. All cases were not indicated for surgery for various reasons. The median age of the patients was 83 years old. A total of 30 or 33 Gy in 10 or 11 fractions was administered. After radiotherapy, 3 patients were able to receive chemotherapy and 13 patients were discharged to home. The median survival time was 108.5 days. One patient suffered cerebral infarction and became bedridden just after advanced gastric cancer with anemia was treated by hemostatic radiotherapy in parallel with rehabilitation. After improvement of activities of daily living, a curative operation was performed. Hemostatic radiotherapy may be a treatment option for advanced gastric cancer with bleeding that is not suitable for resection at the time of diagnosis.
View full abstractDownload PDF (738K) Full view HTML
-
Ichiro Takemasa2021Volume 54Issue 2 Pages E1
Published: 2021
Released on J-STAGE: April 14, 2021
JOURNAL OPEN ACCESSDownload PDF (788K)
-
Ichiro TakemasaArticle type: EDITOR'S NOTE
2021Volume 54Issue 2 Pages en2-
Published: February 01, 2021
Released on J-STAGE: February 26, 2021
JOURNAL OPEN ACCESS FULL-TEXT HTMLDownload PDF (194K) Full view HTML
- |<
- <
- 1
- >
- >|