
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Kimihiko Funahashi, Michio Itabashi, Yoshito Akagi, Keiji Koda, Koutar ...Article type: ORIGINAL ARTICLE
2019Volume 52Issue 10 Pages 551-563
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLPurpose: The aim of this study was to analyze the current status of intersphincteric resection (ISR) for lower rectal cancer and the issue of post-resection anorectal dysfunction in Japan, based on the results of a questionnaire. Materials and Methods: A questionnaire was distributed to 441 facilities in Japan approved by the Japan Society of Coloproctology. Result: The response rate was 39% (172 facilities). Eighty-eight (51%) facilities performed ISR procedures during the survey period. In 62/88 (70%) facilities, less than 5 patients underwent an ISR procedure. A diverting stoma was created following ISR in almost all of the facilities. In 52% of 142 responding facilities, the diverting stoma could not be reversed because of issues including recurrence, problems associated with anastomosis, and anal sphincter-related dysfunction; thus, a permanent stoma remained. In addition, about 90% of 142 responding facilities reported that patients had anorectal dysfunction, even though they were followed for over 2 years after diverting stoma reversal. In 81% of the facilities, patients had fecal incontinence. Fecal incontinence after ISR was associated with resection volume of the internal anal sphincter muscle, anastomosis-related issues, age, radiation therapy, and gender. Most of the responding facilities reported that 20%–30% of patients who underwent ISR had fecal incontinence, followed by 50%, almost all, and 70%–80%, with frequencies of 41%, 20%, 12%, and 8%, respectively. Regarding treatment of anorectal dysfunction, the surgeon alone provided treatment in almost all facilities. Many patients were treated with medication, although various treatments were used. Conclusion: This survey analysis found that patients in many facilities had a diverting stoma that could not be reversed after ISR, and in some patients, severe anorectal dysfunction occurred after ISR. Surgeons should understand the risks associated with an ISR procedure, including the possibility of anorectal dysfunction following ISR. When choosing an ISR procedure for lower rectal cancer, surgeons must perform the procedure properly, upon obtaining informed consent.
View full abstractDownload PDF (1555K) Full view HTML
-
Yasuhiro Shimizu, Jun Kimura, Hirochika Makino, Atsushi Ishibe, Hiroto ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 564-571
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLA 49-year-old man underwent total gastrectomy with lower esophageal resection and Roux-en Y reconstruction after 2 courses of DCS therapy for stage III esophagogastric junctional cancer. Suture failure of the esophago-jejunostomy occurred on postoperative day (POD) 5, and bloody drainage was observed from the anastomotic drain on the same day. On POD10, a large amount of hematemesis was noted, resulting in hemorrhagic shock, so emergency operation was performed. A perforation of about 10 mm in the descending aorta on the dorsal side of the anastomosis was found, and hemostasis was achieved with gauze packing. On POD11, endovascular aneurysm repair (EVAR) was performed, and no bleeding was observed. Esophagectomy was performed on POD12, and esophageal reconstruction using the jejunum was performed 6 months later. After the operation, suture failure was observed. However, about 3 months later, the fistula closed and the patient was discharged. Although EVAR is usually used for the treatment of aortic aneurysm, it can also be used for aorto-esophageal fistula after surgery for upper gastrointestinal tract.
View full abstractDownload PDF (1760K) Full view HTML -
Kenta Baba, Masaru Sasaki, Kensuke Shimbara, Tatsuya Tazaki, Yoichi Su ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 572-581
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLA 52-year-old woman was admitted to our hospital with a diagnosis of breast cancer and was evaluated in our Department of Breast Surgery. Abdominal US showed a mass in the hepatic hilum. A CT scan and MRI revealed a 20-mm mass adjacent to the cystic duct. A PET scan showed an accumulation of FDG based on the location of the mass and the standardized uptake value was 3.5. Although ERCP showed compression in the cystic duct, there was no interruption and the gallbladder was visualized. The imaging findings were atypical for a cholangiocarcinoma. The differential diagnosis included non-epithelial tumors of the gallbladder or cystic duct, and lymphadenopathy. The possibility of malignant disease could not be ruled out; thus we performed an extended cholecystectomy with resection of the bile duct. Macroscopically, the mass was well-defined, solid, and bordered the cystic duct. The histopathologic examination showed that the tumor occurred between the submucosa and serosa of the cystic duct and had spindle-shaped cells with a palisading pattern. Immunohistochemical studies revealed S-100 protein positivity. Taken together, we made a diagnosis of a schwannoma arising from the cystic duct.
 View full abstractDownload PDF (2200K) Full view HTML
View full abstractDownload PDF (2200K) Full view HTML -
Tomohiro Okura, Takefumi Niguma, Toru Kojima, Nobuyuki Watanabe, Souic ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 582-589
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLA 76-year-old woman underwent a pancreaticoduodenectomy for carcinoma in the head of the pancreas. The pathological diagnosis was spindle cell type anaplastic carcinoma. After the operation, she received adjuvant chemotherapy, and she had been followed recurrence-free for 10 years. When she was 86 years old, CEA was increased and dynamic abdominal CT scan revealed a 30 mm tumor in the remnant pancreas and a dilated main pancreatic duct. Adenocarcinoma was diagnosed by biopsy of the tumor under endoscopic ultrasound-guided fine needle aspiration, and total remnant pancreatectomy was performed. The pathological diagnosis was moderately differentiated type of invasive ductal carcinoma. Anaplastic carcinoma of the pancreas is a rare type of invasive ductal carcinoma, and to the best of our knowledge, only a few cases of long survival over 10 years have been reported in Japan.
View full abstractDownload PDF (1909K) Full view HTML -
Hiroyuki Fukuda, Tomohisa Okaya, Hidehito Shibasaki, Hirokazu Karaki, ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 590-598
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
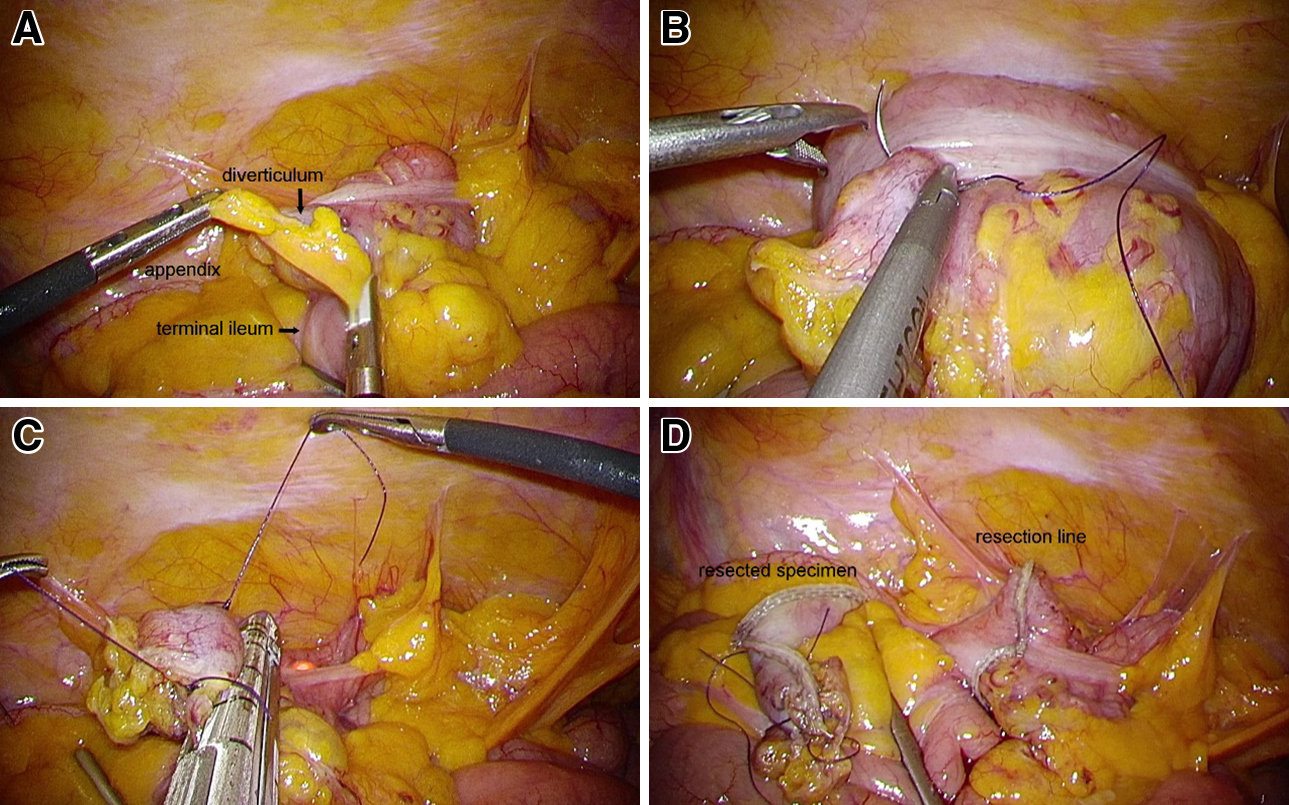
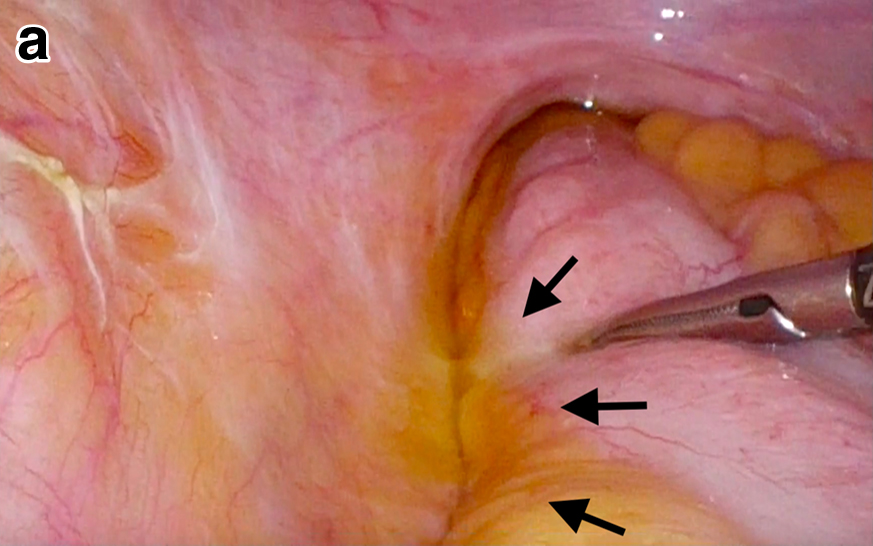
JOURNAL FREE ACCESS FULL-TEXT HTMLA 77-year-old man who has been treated by endoscopic hemostasis for frequent rebleeding of colonic diverticula for four years, underwent elective laparoscopic surgery. First, intraoperative colonoscopy was performed to identify the culprit diverticulum, to which several endoscopic hemostatic clips had been applied preoperatively. Then, the culprit diverticulum was sutured laparoscopically under the observation of colonoscopy, and local resection was performed by endoscopic linear stapler while the sutured strings were pulled up by grasping forceps. He was discharged with good postoperative course and has been followed up one-year after surgery. Japanese guidelines for the management of colonic diverticulosis (diverticular bleeding, diverticulitis) established by the Japanese Gastrointesitinal Association recommends colectomy for diverticular bleeding resistant to endoscopic hemostasis and interventional radiology, following the preoperative bleeding source identification. We propose it is desirable to reduce the extent of colectomy and counteract the surgical stress, because colonic diverticulum is a benign disease. The present procedure may have benefits such as reduction of operative risks and avoidance of massive colectomy. To the best of our knowledge, no similar cases have previously been reported in the literature.
 View full abstractDownload PDF (1675K) Full view HTML
View full abstractDownload PDF (1675K) Full view HTML -
Takahiko Tanigawa, Akira Ishikawa, Tomohiro Mori, Ichiro Higuchi, Yous ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 599-604
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLA 63-year-old man with rectal cancer underwent laparoscopic anterior resection with D3 lymph node dissection in November 2015. Postoperative irradiation (50 Gy) combined with capecitabine and 2 courses of adjuvant chemotherapy with capecitabine plus oxaliplatin was added. One year and 9 months after surgery, a local recurrence of 2 cm was observed on the left front side of the sacrum. For radical cure, it was considered that low anterior resection with concomitant sacral resection was necessary, but as a result of informed consent, carbon ion radiotherapy was selected at the request of the patient. The tumor was in close proximity to the colon, and laparoscopic anterior resection was performed after one month of carbon ion radiotherapy (73.6 Gy). Spacer insertion surgery has been reported as a method to secure the safety margin of tumors and high radiation sensitive organs to reduce the exposure during carbon ion radiotherapy. The radiation exposed colon resection has three advantages: (1) the carbon ion radiotherapy can be started promptly because the operation is performed after irradiation; (2) it is considered that complications such as infection and allergies are less likely to occur compared with spacer insertion surgery using artificial objects; (3) the radiation exposed colon resection may be able to remove secondary lymph node metastasis from recurrent tumors. The radiation exposed bowel resection was considered to be useful for expanding the indication of carbon ion radiotherapy.
 View full abstractDownload PDF (1403K) Full view HTML
View full abstractDownload PDF (1403K) Full view HTML -
Shinsei Matsuoka, Takashi Ishida, Koji Okabayashi, Masashi Tsuruta, Ta ...Article type: CASE REPORT
2019Volume 52Issue 10 Pages 605-610
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLWe encountered a 39-year-old man who was given a diagnosis of solitary fibrous tumor and underwent radical cystoprostatectomy and urinary tract change (preparation of a neobladder). A small bowel obstruction appeared on postoperative day 12; intestinal radiography and abdominal CT revealed that the obstruction was caused by the left urinary tract. We re-operated on postoperative day 22 to release the obstruction. In the operative view, the left urinary tract was exposed to the left colic gutter and looped. One meter of small intestine had invaginated into the loop, but no significant bowel ischemia or gangrene was found. After releasing the internal hernia, we covered the exposed urinary tract with omental fat to prevent hernia recurrence. The postoperative course was uneventful. An internal hernia caused by the urinary tract is very rare.
View full abstractDownload PDF (1480K) Full view HTML
-
Hirokazu NoshiroArticle type: EDITOR'S NOTE
2019Volume 52Issue 10 Pages en10-
Published: October 01, 2019
Released on J-STAGE: October 29, 2019
JOURNAL FREE ACCESS FULL-TEXT HTMLDownload PDF (644K) Full view HTML
- |<
- <
- 1
- >
- >|