
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Toshimichi Tanaka, Heita Ozawa, Teppei Miyakawa, Hiroki Nakanishi, Aki ...Article type: ORIGINAL ARTICLE
2020Volume 53Issue 12 Pages 945-951
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLPurpose: In stoma closure, a combination of circular skin suture and negative pressure wound therapy is likely to reduce surgical site infection (SSI). The aim of the study was to examine the effectiveness of negative pressure wound therapy in stoma closure. Materials and Methods: A retrospective study was performed for 52 patients who underwent stoma closure from August 2015 to July 2018. Postoperative short-term outcomes (surface SSI, organ space SSI, intestinal obstruction, postoperative hospital stay) were compared by classifying the patients into those who underwent circular skin suture alone (group K, n=20) and those treated with circular skin suture and PICO® (group KP, n=32). Results: The rate of superficial incisional SSI differed significantly between groups K and KP (10% vs. 0%, P=0.047). There were no significant differences between the groups in operation time, blood loss, and postoperative hospital stay. Group K was an independent risk factor for SSIs in stoma closure (P=0.047). Conclusion: In stoma closure, combining PICO® with circular skin suture may be effect for further prevention of SSIs.
View full abstractDownload PDF (1089K) Full view HTML
-
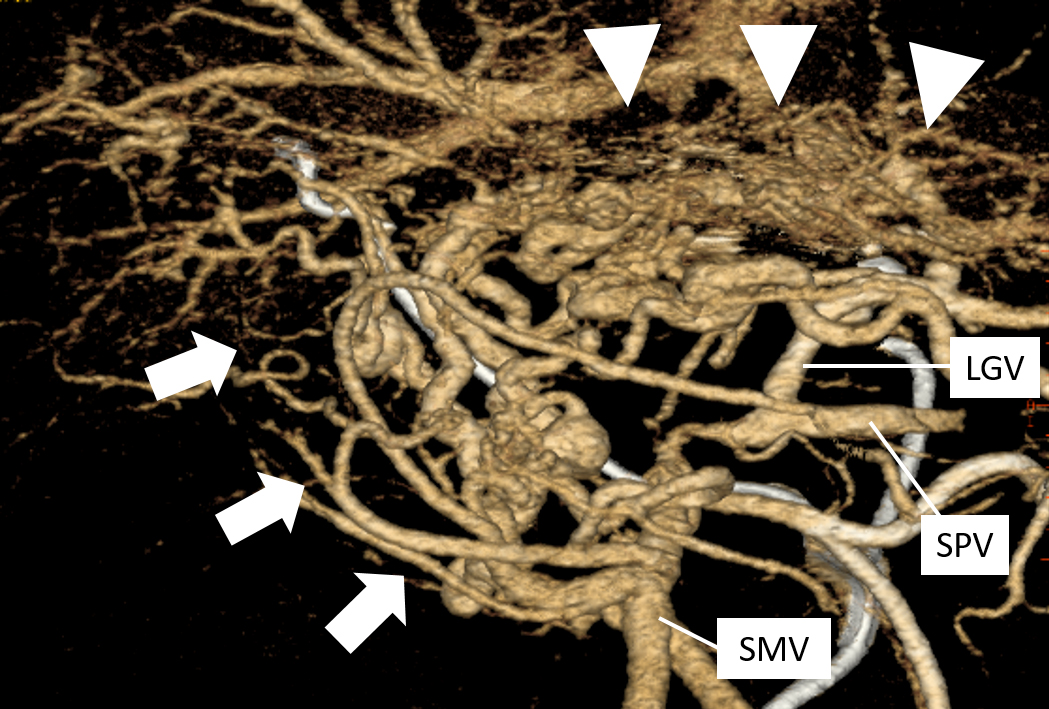
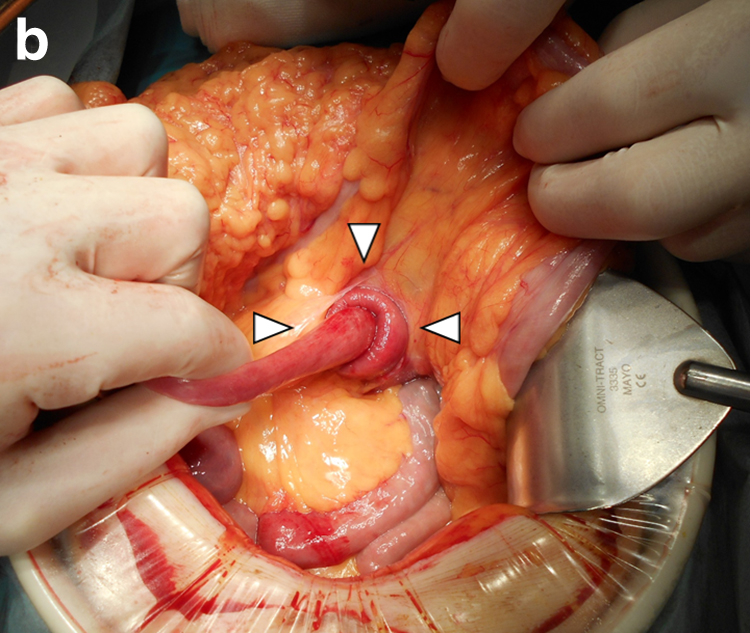
Hirochika Kato, Takashi Ishida, Yoshifumi Ikeda, Takashi Oyama, Nobuhi ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 952-959
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 71-year-old male with alcoholic liver cirrhosis complained of melena during systemic chemotherapy for hepatocellular carcinoma. Upper gastrointestinal endoscopy revealed venous bleeding from an erosion in the gastric pylorus. Abdominal contrast-enhanced CT and angiography revealed tumor thrombosis in the main portal vein and collateral vessels of the lesser omentum, which we diagnosed as portal hypertensive gastropathy (PHG). Endoscopic hemostasis did not completely stop the bleeding and frequent blood transfusions were required. The esophageal/gastric varices were not highly developed and did not bleed; the bleeding site was located in the gastric pylorus. Thus, distal gastrectomy was performed. We maximally preserved the collateral vessels to maintain hemodynamics. Bleeding did not recur in the 6-month period following the operation. This is the first report of successful use of distal gastrectomy to treat refractory gastric hemorrhage in a patient with PHG.
 View full abstractDownload PDF (1574K) Full view HTML
View full abstractDownload PDF (1574K) Full view HTML -
Kei Kawashima, Sho Sato, Atsushi Ishibe, Takashi Kosaka, Nobuhiro Tsuc ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 960-967
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 62-year-old male presented with fever lasting for 5 days, vomiting, and diarrhea. Abdominal enhanced CT revealed intraperitoneal gas around the duodenum and abscess formation extending throughout the retroperitoneal space from the posterior of the duodenum into the pelvic. These findings led to a diagnosis of retroperitoneal abscess with duodenal ulcer penetration. Treatment with percutaneous drainage and antibiotics was used. CT-guided drainage of the abscess cavity of the right pelvic region was performed on the 3rd hospital day. Exchange of the drainage tube was needed several times because the abscess cavity was extensive, but the drainage was effective. An upper gastrointestinal series performed on the 21st hospital day showed closure of the penetration site, and oral intake was started on the same day. X-ray fluoroscopy performed on the 42nd hospital day indicated complete resolution of the abscess cavity, and the drainage tube was removed. The patient was discharged on the 45th hospital day. Conservative management for penetrating duodenal ulcer with retroperitoneal abscess formation is less invasive than surgery and may be a treatment option for patients with stable vital signs.
View full abstractDownload PDF (1330K) Full view HTML -
Kazuki Higure, Takao Ide, Hirokazu NoshiroArticle type: CASE REPORT
2020Volume 53Issue 12 Pages 968-975
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLThe patient was a 49-year-old man with a history of several treatments for hepatocellular carcinoma by radiofrequency ablations and transcatheter arterial chemoembolization. He was admitted to our hospital with obstructive jaundice (T-bil 16.2 mg/dl) and he had multiple tumors in the right hepatic lobe. A CT scan showed that the right hepatic lobe, colon, small intestine and duodenum were elevated into the right pleural cavity, and dilatation of the intrahepatic bile duct was revealed. After reduction of jaundice by endoscopic nasobiliary drainage, right lobectomy was performed for recurrence of hepatocellular carcinoma and simultaneous repair of diaphragmatic hernia. The present case is an extremely rare report of incarcerated diaphragmatic hernia with obstructive jaundice after radiofrequency ablation.
 View full abstractDownload PDF (1911K) Full view HTML
View full abstractDownload PDF (1911K) Full view HTML -
Yudai Hojo, Yoshiharu Shirakata, Ai Izumi, Jun Matsui, Tokuyuki Yamash ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 976-984
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 45-year-old woman was referred to our department with a diagnosis of appendiceal cancer. Contrast enhanced CT revealed a 20 mm appendiceal mass that showed high FDG accumulation on FDG-PET/CT. Lower gastrointestinal endoscopy demonstrated a protruding lesion in the appendiceal orifice, but no neoplastic changes were found in biopsy specimens. Laparoscopic ileocecal resection was performed. Histopathological examination showed dense fibrosis and lymphoplasmacytic infiltration in the appendiceal mass. The number of IgG4-positive plasma cells was 112/HPF and the IgG4-positive/IgG-positive plasma cell ratio was 78.3%; therefore, IgG4-related inflammatory pseudotumor was suspected. However, there were some atypical points in this case for diagnosis of IgG4-related disease: focal inflammatory cell infiltration, the presence of neutrophilic infiltration and granulation tissue, and the absence of elevated serum IgG4 concentrations and other organ involvement. Further analysis of similar cases is needed to determine if this appendiceal lesion is truly IgG4-related disease.
View full abstractDownload PDF (1641K) Full view HTML -
Ryuta Ueda, Hirofumi Kon, Yosuke Wakui, Toshihiro Sakata, Daisuke Kura ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 985-991
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLThe patient was a 63-year-old male who had been on hemodialysis for 19 years because of end-stage renal failure due to diabetic nephropathy and who had been taking oral calcium polystyrene sulfonate (CPS) as a treatment for hyperkalemia. Previously, he underwent detailed tests for progressive anemia and black stools, and was diagnosed with descending colon cancer, for which he was treated by laparoscopic segmental colectomy of the descending colon with D3 lymphadenectomy. The postoperative course was uneventful and the patient was discharged on hospital day 11. However, because subsequent findings revealed progressive anemia and recurrence of bloody stools, lower gastrointestinal endoscopy was performed on hospital day 43. A bleeding circumferential ulcer was found at the anastomotic site and a longitudinal ulcer was detected at a different site. Biopsy of the ulcers revealed basophilic rhomboid deposits on the ulcer floor; thus, involvement of CPS was suspected. Hence, oral administration of CPS was discontinued, and as a result, anemia ceased to progress and subsequent lower gastrointestinal endoscopy showed improvement of the ulcers. Three years have passed and the patient has survived without recurrence of cancer or ulcers.
 View full abstractDownload PDF (1487K) Full view HTML
View full abstractDownload PDF (1487K) Full view HTML -
Yusuke Murase, Nobuhisa Matsuhashi, Takao Takahashi, Yoshinori Iwata, ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 992-1001
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLA 57-year-old woman was admitted to our hospital because of erythema on the right side of her anus. A skin biopsy showed Paget cells in the epidermis, and immunohistochemical staining revealed pagetoid spread of anal canal cancer. Although colonoscopy showed no mass lesions in the rectum and step biopsy was negative, mapping biopsy from the anal mucosa was positive. Therefore, we thought it necessary to remove the lesion, including the skin near the anus, to obtain curative resection. There was no evidence of infiltration to the muscularis propria, and we thought that resection in the submucosal layer would ensure a radical cure and preserve anal function. ESD, trans-anal submucosal resection, and cutaneous malignant tumor resection were performed jointly by gastrointestinal surgery, gastroenterology, and dermatology surgeons, respectively. The patient was discharged from hospital 17 days after surgery. In this case of anal canal cancer with pagetoid spread, abdominoperineal rectal resection was avoided and anal function was preserved. We report this relatively rare case including our surgery and the progress of the patient.
View full abstractDownload PDF (1718K) Full view HTML -
Tetsuo Tsukahara, Eiji Hayashi, Takeo Kawahara, Hiroki Aoyama, Tetsuro ...Article type: CASE REPORT
2020Volume 53Issue 12 Pages 1002-1008
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLAn 87-year-old woman with no history of abdominal surgery visited our hospital because of frequent vomiting. Since abdominal plain CT revealed gastric distension, the jejunum intussuscepted into the duodenum in a retrograde fashion and a mass was formed by the small intestine around the ligament of Treitz. An emergency laparotomy was performed for a suspected jejunal internal hernia accompanied by retrograde intussusception. Operative findings showed a 15-cm portion of the most proximal jejunum to be herniated and incarcerated in the transverse mesocolon through an orifice 2 cm in diameter formed at the mesocolic fossa. The invaginated intestine was reverted manually and had no necrosis. Intraoperative esophagogastroduodenoscopy revealed no neoplastic lesions, so the orifice was closed by suture. The postoperative course was uneventful. We report this rare case of transverse mesocolon hernia into the mesocolic fossa accompanied by retrograde intussusception.
 View full abstractDownload PDF (1390K) Full view HTML
View full abstractDownload PDF (1390K) Full view HTML
-
Taizo HibiArticle type: SPECIAL REPORT
2020Volume 53Issue 12 Pages 1009-1015
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTML -
Tomomichi KiyomatsuArticle type: SPECIAL REPORT
2020Volume 53Issue 12 Pages 1016-1025
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTML
-
Seiichiro YamamotoArticle type: EDITOR'S NOTE
2020Volume 53Issue 12 Pages en12-
Published: December 01, 2020
Released on J-STAGE: December 26, 2020
JOURNAL OPEN ACCESS FULL-TEXT HTMLDownload PDF (803K) Full view HTML
- |<
- <
- 1
- >
- >|