
- Issue 12 Pages 695-
- Issue 11 Pages 611-
- Issue 10 Pages 551-
- Issue 9 Pages 485-
- Issue 8 Pages 405-
- Issue 7 Pages 345-
- Issue 6 Pages 281-
- Issue 5 Pages 239-
- Issue 4 Pages 191-
- Issue 3 Pages 137-
- Issue 2 Pages 83-
- Issue 1 Pages 1-
- Issue Special_Issue P・・・
- Issue Supplement2 Pag・・・
- Issue Supplement1 Pag・・・
- |<
- <
- 1
- >
- >|
-
Eiichi Nakao, Akira Watanabe, Tetsuo Abe, Hidetaka Ono, Hiroyuki Baba, ...Article type: ORIGINAL ARTICLE
2020 Volume 53 Issue 2 Pages 125-130
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLPurpose: While the discontinuation of antithrombotic medications decreases bleeding during operations and postoperatively, it nevertheless carries a substantial risk for thromboembolic events. According to the guidelines for management of anticoagulant and antiplatelet therapy in cardiovascular disease, a “small operation of body surface with continued treatment with warfarin and antiplatelet therapy when it is easy to respond to postoperative bleeding” is recommended in class IIa'. In our hospital, we have performed inguinal hernia repair by anterior approach method in patients undergoing continued antithrombotic therapy. We examined the safety of this operation. Materials and Methods: A total of 242 patients who underwent anterior approach method for inguinal hernia between April 2014 and March 2017 were included in the analysis. We excluded bilateral, children, laparoscopic surgery, recurrent cases, and incarcerated cases. We divided patients into the group undergoing antithrombotic therapy, and the group without antithrombotic agent administration, and compared patient characteristics and surgical outcomes. Result: Of the 242 patients, 66 patients were receiving antithrombotic therapy (antithrombotic group), and 176 patients were not receiving antithrombotic therapy (control group). The antithrombotic group had a greater mean age and had higher ASA scores, PT-INR scores. Furthermore, a greater number of patients from this group had comorbidity. There were no significant differences in intra and postoperative bleeding between the two groups. Conclusion: Inguinal hernia repair by anterior approach method can be safely performed in patients who continue to receive antithrombotic agents.
View full abstractDownload PDF (1056K) Full view HTML
-
Tomoyuki Kakuta, Satoru Nakagawa, Takeo Bamba, Masaki Aizawa, Atsushi ...Article type: CASE REPORT
2020 Volume 53 Issue 2 Pages 131-138
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLA 69-year-old woman, with a diagnosis of poorly differentiated squamous cell carcinoma of thoracic esophagus (T3N2M0, Stage III, UICC 7th), underwent right thoracic esophagectomy with three-field lymphadenectomy following neoadjuvant chemotherapy. At 9 months after esophagectomy, she underwent definitive chemo-radiotherapy for a recurrence of mediastinal lymph nodes. In the follow-up course, abdominal CT scan at 2 years and 2 months after esophagectomy revealed an enhanced mass in the left adrenal region, diagnosed as adrenal metastasis. The tumor shrank noticeably owning to a continuous chemotherapy; however, showed a regrowth after interruption of chemotherapy. PET/CT scan showed high accumulation of FDG in the left adrenal region, with no other obvious accumulations including the mediastinum. Surgical resection for the left adrenal gland was performed at 4 years after esophagectomy. She was periodically followed up without any additional treatment, and survived for 10 years after esophagectomy and 6 years after the last surgery without any recurrence of disease. Although the prognosis of hematogenous recurrences after radical esophagectomy is considered to be poor, this case suggests a benefit of surgical resection for a solitary metastasis of esophageal carcinoma.
View full abstractDownload PDF (1544K) Full view HTML -
Kenta Nishitani, Hirohisa Kitagawa, Kazuyuki KawamotoArticle type: CASE REPORT
2020 Volume 53 Issue 2 Pages 139-146
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLNeuroendocrine tumors (NETs) of the gastrointestinal tract, pancreas, and liver are very rare. We report a case of primary hepatic NET. The patient was a 74-year-old man who had undergone left renal pelvis carcinoma surgery, in whom liver metastasis in segment 7 was detected by follow-up CT. We performed a liver biopsy and a NET was diagnosed. We performed radiofrequency ablation (RFA) on segment 7 of the liver. Nine months later, he had a recurrence of liver cancer (segment 4: two sites, segment 5: one site), for which we performed transcatheter arterial chemoembolization. Eighteen months later, both lesions enlarged, and we performed RFA on segment 5. The two sites in segment 4 were difficult to treat by RFA, therefore a laparoscopic liver partial resection was performed. The postoperative pathological diagnosis was NET G1 according to the WHO Classification of Tumours of the Digestive System.
View full abstractDownload PDF (2301K) Full view HTML -
Hideyuki Dei, Seiji Natsume, Yoshiki Senda, Masataka Okuno, Daisuke Ha ...Article type: CASE REPORT
2020 Volume 53 Issue 2 Pages 147-153
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
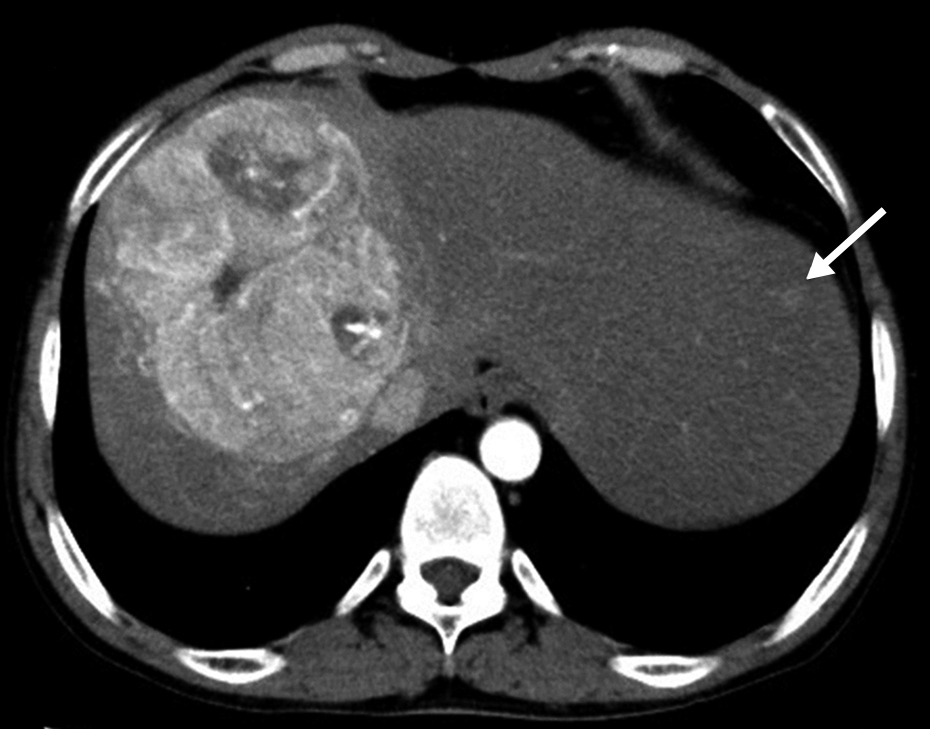
JOURNAL FREE ACCESS FULL-TEXT HTMLIt is extremely rare for hepatocellular carcinomas to occur in patients with glycogen storage disease. Here, such a case is reported. The patient, a 37-year-old man, was given a diagnosis of hepatocellular carcinoma occupying the right lobe, by CT. A diagnosis of glycogen storage disease had been given in his childhood. Because the tumor extended to the orifice of right, middle hepatic vein, and inferior vena cava, and was considered to be unresectable, he underwent transcatheter arterial chemoembolization. As a result, the size of the tumor was reduced from 11 cm to 7 cm. Right hepatectomy was performed. The volume of blood loss was 850 ml, and the operative time was 493 minutes. The patient experienced two postoperative complications possibly due to his glycogen storage disease. Severe lactic acidosis was treated with high concentration glucose administration on the 2nd postoperative day. Moreover, intraperitoneal bleeding from bilateral inferior phrenic arteries possibly due to the thrombocyte malfunction was stopped with transcatheter arterial embolization on the 6th postoperative day.
 View full abstractDownload PDF (1386K) Full view HTML
View full abstractDownload PDF (1386K) Full view HTML -
Kunihiko Tsuboi, Yoko Shono, Yoo Lee, Masahiko Okamura, Yo Mizukami, T ...Article type: CASE REPORT
2020 Volume 53 Issue 2 Pages 154-163
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLA 15-year-old adolescent girl was transported to our hospital because of abdominal pain and vomiting. Abdominal CT showed coprostasis in the rectum and the sigmoid colon. The small and large intestine were markedly extended and filled with content fluid. Colonoscopy with intestinal lavage showed the mucosa of the sigmoid colon turning purplish or blackish. Under the diagnosis of stercoral obstructive colitis with colonic ischemia, emergency laparotomy was performed. The colon was studded with spotty ischemic changes. Removal of feces and irrigation in the colon with intraoperative colonoscopy improved the mucosal appearance. Total colon was preserved and diverting ileostomy was performed. Intensive care after surgery improved her general status. Colonoscopy with enema on day 25 and day 85 showed severe stenosis at the right side of the transverse colon and the lead-pipe appearance from the left side of the transverse colon to the descending colon. Irreversible colonic stenosis was suspected, and subtotal colectomy was performed on day 103. The resected colon was compatible with ischemic colitis by the naked eye and histopathologically. After ileostomy closure on day 138, she returned to her school life. We report the youngest case of stercoral obstructive colitis in Japan with a literature review of 20 cases.
 View full abstractDownload PDF (1754K) Full view HTML
View full abstractDownload PDF (1754K) Full view HTML -
Ryosuke Fukuyo, Hironobu Baba, Takatoshi Matsuyama, Akifumi Kikuchi, S ...Article type: CASE REPORT
2020 Volume 53 Issue 2 Pages 164-171
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLSince the Japanese insurance system initiated coverage of robotic proctectomy, the number of procedures performed and their importance are gradually increasing. Robotic colectomy is also increasingly reported worldwide, but not in Japan. We herein report two cases of robotic right colectomy utilizing the da Vinci surgical system Xi® for the first time in Japan. D3 lymphadenectomy and right colon mobilization was performed with the placement of four trocars in line with and above the pubic tubercle, and intra-corporeal anastomosis was performed using SureForm®. Both patients were discharged on postoperative day 6 without any complications. It has been reported that robotic colectomy requires a longer operation time than that required for conventional laparoscopic colectomy, but the estimated blood loss, complications, and pain after surgery may be decreased. To confirm the safety and curability of robotic colectomy, further studies and case encounters are needed.
View full abstractDownload PDF (2467K) Full view HTML -
Yoshiro Hayashi, Kosuke Oishi, Satoru Huruhashi, Koichi Nakamura, Taka ...Article type: CASE REPORT
2020 Volume 53 Issue 2 Pages 172-180
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLHere, we present the case of a 68-year-old man who underwent laparoscopic low anterior resection for overlap cancer of the sigmoid colon and rectum. After surgery, anastomotic leakage led to peritonitis and abdominal abscess, for which a colostomy was constructed in the transverse colon. Three months after he was discharged with preservative treatment by drainage, complete obstruction of the rectal anastomotic site was confirmed by an enema examination. Tuberculosis was simultaneously detected and treated, and it was decided to attempt the closure of the colostomy and the release obstruction of the intestinal anastomotic part. However, in this case, endoscopic incision or reoperation seemed difficult. Therefore, a magnet-compressed anastomotic stenosis restriction surgery (second Yamauchi method) was performed. After approximately 4 years after this surgery, the opening of the rectal anastomotic site is still maintained. This method is thus considered an effective means for refractory gastrointestinal stricture/obstruction with least medical invasion.
View full abstractDownload PDF (2401K) Full view HTML
-
Shoichi Irie, Akio SaiuraArticle type: SPECIAL REPORT
2020 Volume 53 Issue 2 Pages 181-188
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTML -
Yuhki Sakuraoka, Keiichi KubotaArticle type: SPECIAL REPORT
2020 Volume 53 Issue 2 Pages 189-197
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTML -
Emi Akizuki, Ichiro TakemasaArticle type: SPECIAL REPORT
2020 Volume 53 Issue 2 Pages 198-204
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTML -
Yutaro Kikuchi, Hirofumi ShirakawaArticle type: SPECIAL REPORT
2020 Volume 53 Issue 2 Pages 205-212
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTML
-
Takashi AkiyoshiArticle type: EDITOR'S NOTE
2020 Volume 53 Issue 2 Pages en2-
Published: February 01, 2020
Released on J-STAGE: February 29, 2020
JOURNAL FREE ACCESS FULL-TEXT HTMLDownload PDF (671K) Full view HTML
- |<
- <
- 1
- >
- >|