Volume 3, Issue 4
Displaying 1-18 of 18 articles from this issue
- |<
- <
- 1
- >
- >|
ORIGINAL ARTICLE
-
2019Volume 3Issue 4 Pages 277-284
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: May 31, 2019Download PDF (513K) -
2019Volume 3Issue 4 Pages 285-294
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: May 31, 2019Download PDF (1342K) -
2019Volume 3Issue 4 Pages 295-303
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: June 21, 2019Download PDF (2176K) -
2019Volume 3Issue 4 Pages 304-311
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: July 10, 2019Download PDF (379K) -
2019Volume 3Issue 4 Pages 312-318
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: August 16, 2019Download PDF (386K) -
2019Volume 3Issue 4 Pages 319-326
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: February 28, 2019Download PDF (218K) -
2019Volume 3Issue 4 Pages 327-334
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: December 28, 2018Download PDF (1371K) -
2019Volume 3Issue 4 Pages 335-341
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: February 28, 2019Download PDF (349K) -
2019Volume 3Issue 4 Pages 342-347
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: February 28, 2019Download PDF (333K) -
2019Volume 3Issue 4 Pages 348-353
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: February 28, 2019Download PDF (591K) -
2019Volume 3Issue 4 Pages 354-360
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: March 22, 2019Download PDF (211K) -
2019Volume 3Issue 4 Pages 361-367
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: March 22, 2019Download PDF (106K) -
2019Volume 3Issue 4 Pages 368-376
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: April 05, 2019Download PDF (1545K) -
2019Volume 3Issue 4 Pages 377-384
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: April 26, 2019Download PDF (485K) -
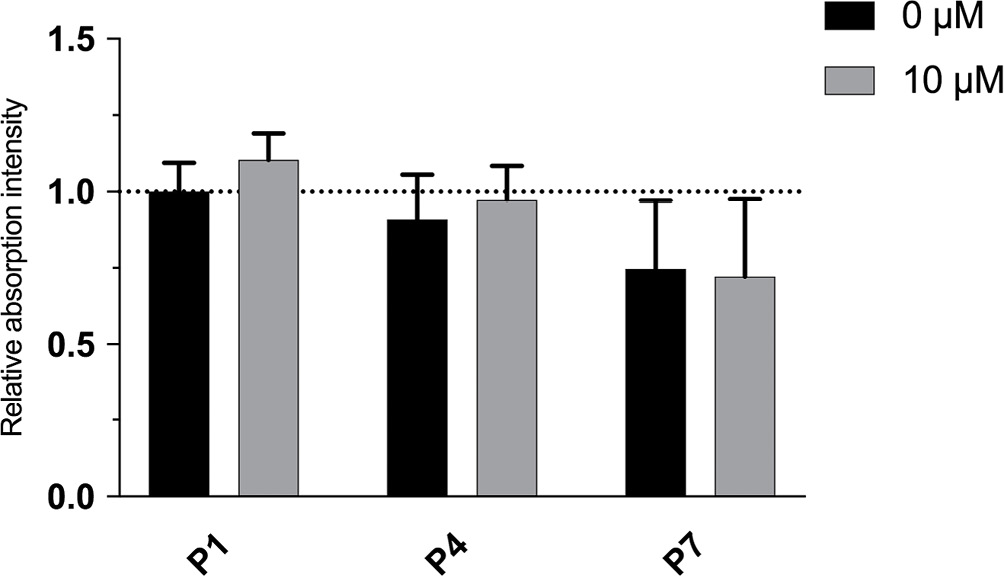
Minimal Sustainability of Dedifferentiation by ROCK Inhibitor on Rat Nucleus Pulposus Cells In Vitro2019Volume 3Issue 4 Pages 385-391
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: August 16, 2019Download PDF (425K)
CASE REPORT
-
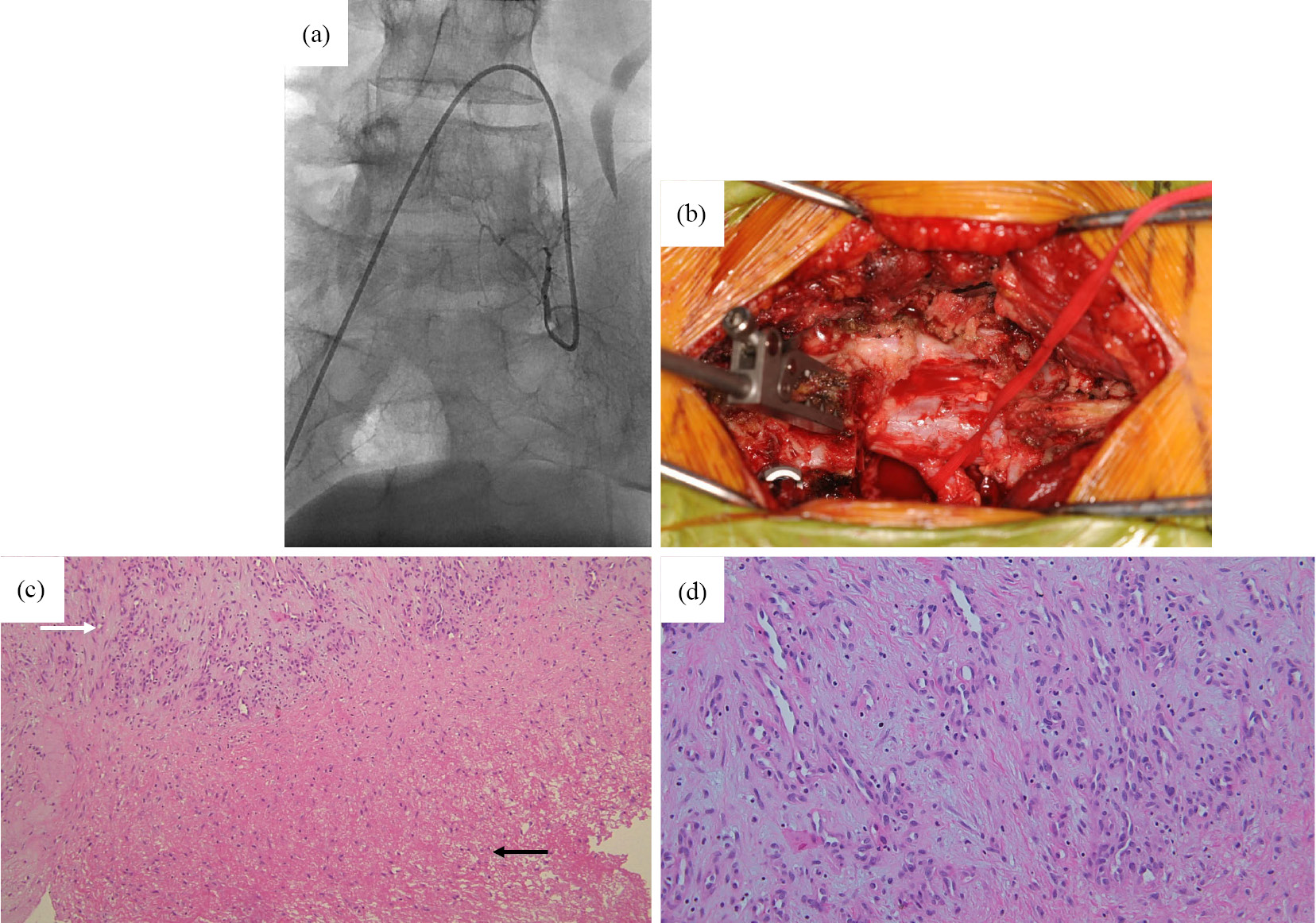
2019Volume 3Issue 4 Pages 392-395
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: October 19, 2018Download PDF (498K)
CLINICAL CORRESPONDENCE
-
2019Volume 3Issue 4 Pages 396-400
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: November 20, 2018Download PDF (1426K) -
2019Volume 3Issue 4 Pages 401-403
Published: October 27, 2019
Released on J-STAGE: October 27, 2019
Advance online publication: December 01, 2018Download PDF (285K)
- |<
- <
- 1
- >
- >|