Volume 2, Issue 4
Displaying 1-15 of 15 articles from this issue
- |<
- <
- 1
- >
- >|
ORIGINAL ARTICLE
-
2018Volume 2Issue 4 Pages 249-252
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (63K) -
2018Volume 2Issue 4 Pages 253-262
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (457K) -
2018Volume 2Issue 4 Pages 263-269
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 07, 2018Download PDF (443K) -
2018Volume 2Issue 4 Pages 270-277
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 07, 2018Download PDF (228K) -
2018Volume 2Issue 4 Pages 278-282
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 07, 2018Download PDF (104K) -
2018Volume 2Issue 4 Pages 283-289
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 07, 2018Download PDF (213K) -
2018Volume 2Issue 4 Pages 290-293
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: March 15, 2018Download PDF (225K) -
2018Volume 2Issue 4 Pages 294-298
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (244K) -
2018Volume 2Issue 4 Pages 299-303
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: May 29, 2018Download PDF (150K) -
2018Volume 2Issue 4 Pages 304-308
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (525K) -
2018Volume 2Issue 4 Pages 309-316
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (1199K) -
2018Volume 2Issue 4 Pages 317-323
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (609K) -
2018Volume 2Issue 4 Pages 324-330
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: May 29, 2018Download PDF (954K)
CASE REPORT
-
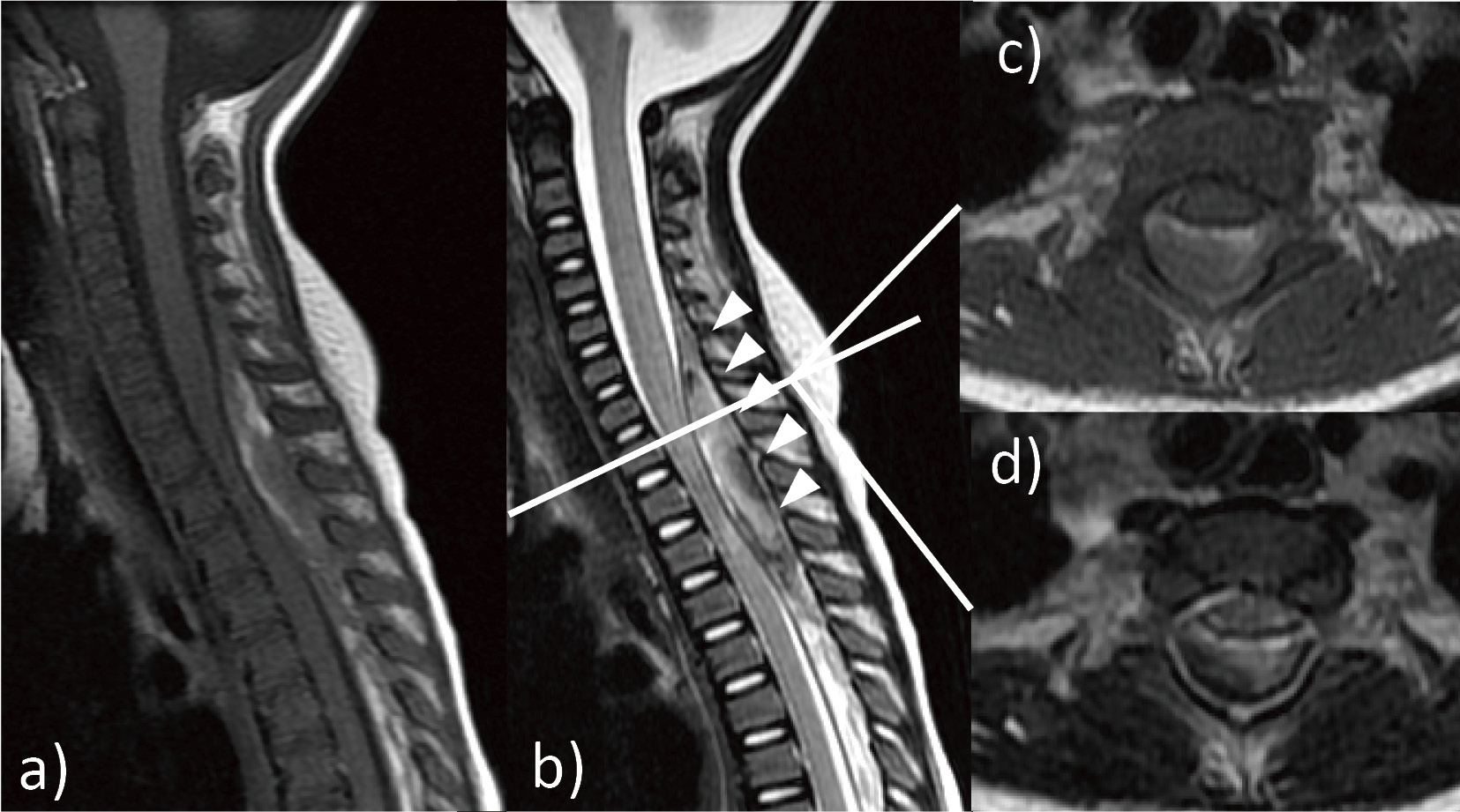
Total Resection of Cervical Ventral Intramedullary Cavernous Hemangiomas with an Anterior Corpectomy2018Volume 2Issue 4 Pages 331-334
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 27, 2018Download PDF (784K) -
2018Volume 2Issue 4 Pages 335-339
Published: October 26, 2018
Released on J-STAGE: October 27, 2018
Advance online publication: April 07, 2018Download PDF (657K)
- |<
- <
- 1
- >
- >|