Introduction: Depending on the underlying cause, fusion may be used as the revision surgery technique following decompression surgery for lumbar canal stenosis or degenerative spondylolisthesis. Posterior lumbar interbody fusion was formerly the main surgical technique used, but oblique lateral interbody fusion (OLIF) is coming into use as a less invasive method. The advantage of OLIF is that it allows minimally invasive and indirect decompression without touching the previous operating field where adhesions and scarring are likely to have developed. In this study, the postoperative outcomes of OLIF were investigated to determine whether it is a suitable approach for revision surgery.
Methods: The study subjects were 16 patients (5 men and 11 women) aged 43-84 years (mean 71 years) at surgery and who underwent OLIF as revision surgery.
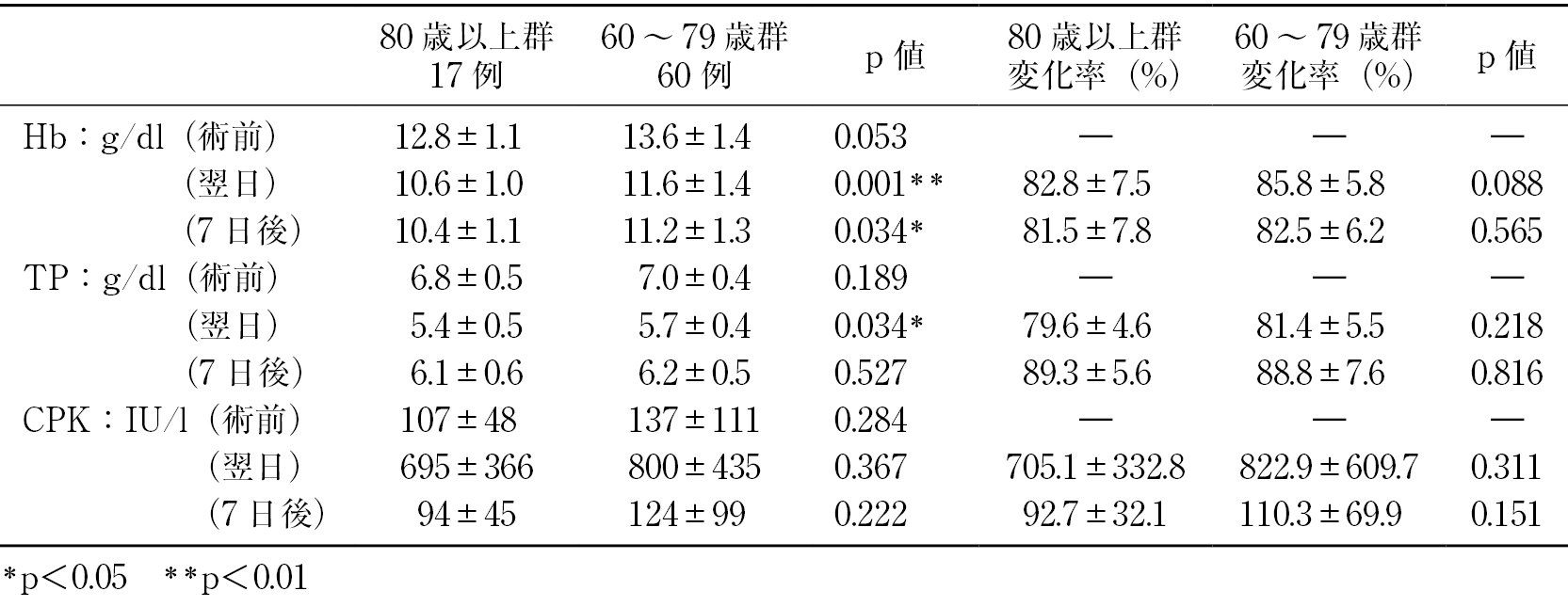
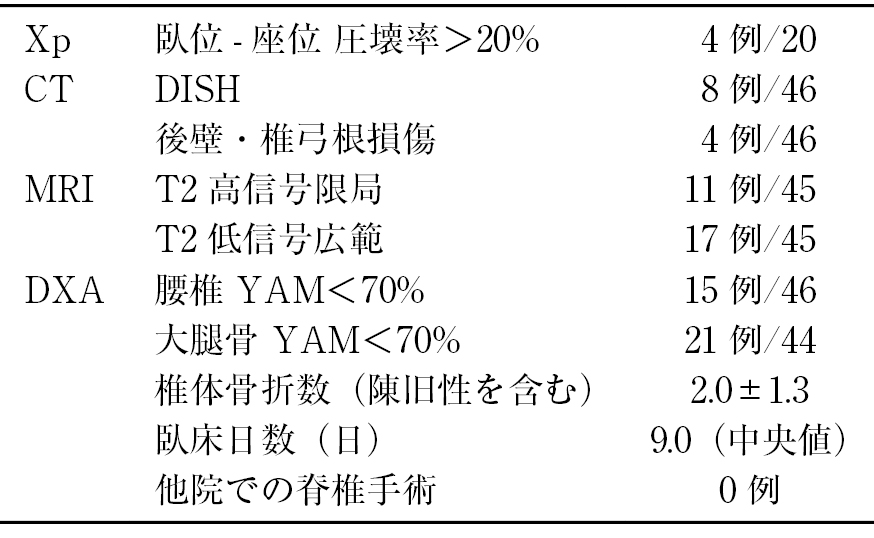
Results: The mean number of back surgeries prior to OLIF was 1.5 (range 1-7). Previous surgeries had been conducted at 10 different hospitals, including our own. The mean time from previous surgery to revision surgery was 5.8 years (range 5 months to 20 years). The number of intervertebral levels treated by OLIF was 1 (n=3 cases), 2 (n=8), and 3 (n=5). The mean operating time was 56 minutes per intervertebral level treated by OLIF, and 87 minutes for posterior pedicle screw (PPS) fusion.
Lower back and lower extremity pain disappeared immediately after surgery. The pre- and post-operative dural tube areas were compared in order to confirm the effectiveness of indirect decompression. The mean preoperative dural tube area was 101 mm2, compared to a mean postoperative dural tube area of 155 mm2.
Synostosis of the fused intervertebral levels was evaluated on coronal/sagittal computed tomography (CT) images and confirmed for all 34 intervertebral levels.
Discussion: OLIF allows indirect decompression without touching operating fields where adhesions may have developed, thus making it possible to carry out corrective fusion. However, further studies are required to determine the clinical outcomes from OLIF in situations such as operating fields with adhesions, or for hernia recurrence. The results of the present study indicate that OLIF was effective in revision surgery.
Conclusions: OLIF was performed as revision surgery following lumbar spinal decompression in 16 patients. This study demonstrated the effectiveness of indirect decompression.
View full abstract