Introduction: A loss of cervical lordosis or kyphotic change after posterior decompression surgery is one of the potential complications when treating patients with cervical spondylotic myelopathy (CSM). K-line in the neck-flexed position (flexion K-line) reflects anterior dynamic compression factors for the spinal cord. Posterior decompression can lead to poor neurological recovery for patients with CSM with flexion K-line (−) than those with flexion K-line (+).
In the present study, the authors aim to compare clinical outcomes and radiographic parameters including sagittal alignment or balance between Group A (flexion K-line [+] and neutral K-line [+]) and Group B (flexion K-line [−] and neutral K-line [+]).
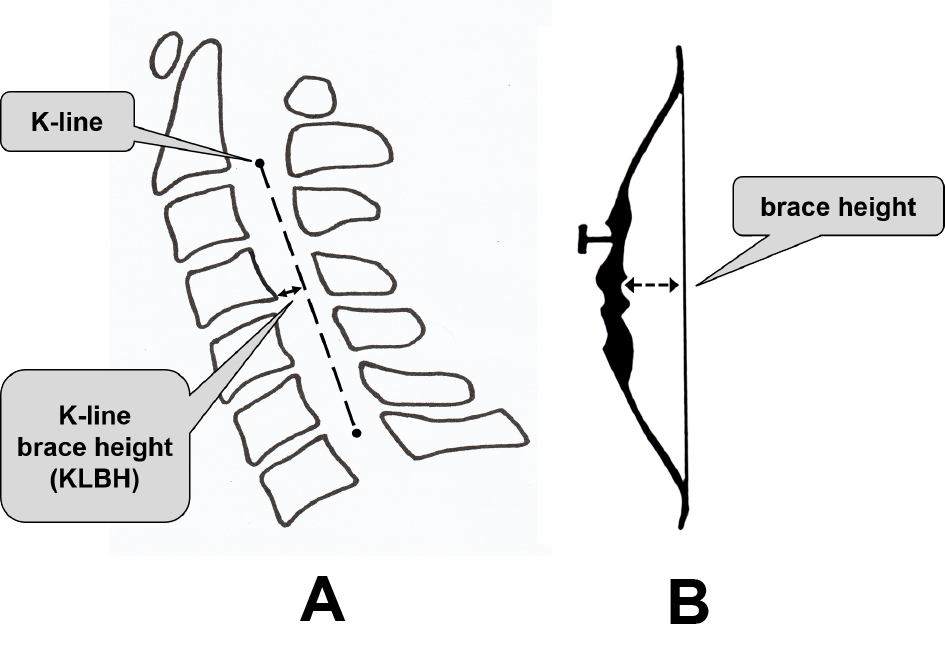
Methods: A total of 42 consecutive patients were enrolled; the inclusion criteria were cases with CSM, posterior decompression surgery, ages 40 or over at the time of surgery, and minimum follow-up period of 6 months. The following radiographic parameters were measured: the minimum distance between K-line and vertebral body or osteophytes (KLBH: K-line brace height), local kyphosis angle, segmental range of motion (ROM), C2-C7 angle, C7 slope, and C2-C7 sagittal vertical axis (SVA). Clinical outcomes were evaluated using the Japanese Orthopaedic Association (JOA) score for cervical myelopathy, JOA Cervical Myelopathy Evaluation Questionnaire, and Visual Analogue Scale. The patients were divided into Group A (n = 31) and Group B (n = 11).
Results: Preoperative KLBH in the flexion, neutral, and extension position and postoperative KLBH in the neutral position were significantly smaller in Group B than in Group A. A postoperative decrease of KLBH in the neutral position was significantly larger in Group B than in Group A. In two cases (4.8%), neutral K-line changed from (+) to (−) after surgery; both cases were in Group B. A postoperative decrease of C2-C7 angle was not significantly different between the two groups. C7 slope and C2-C7 SVA were similar between the two groups. The number of cases with preoperative focal kyphosis angle ≥10° and/or with segmental ROM ≥10° was significantly larger in Group B than in Group A. In addition, MRI findings and clinical outcomes were similar between the two groups.
Conclusions: In patients with CSM, neutral K-line can change from (+) to (−) after posterior decompression. Preoperative flexion K-line (−), focal kyphosis angle ≥10°, and segmental ROM ≥10° are potential risk factors for a loss of cervical lordosis or kyphotic change. With the above factors, additional measures including partial fusion or correction may be required to prevent a loss of cervical lordosis or kyphotic change.
View full abstract